Final ID: Sa2049
Pregnancy Termination or Perinatal Hospice due to Fetal Congenital Heart Defects: A Qualitative Analysis
Abstract Body (Do not enter title and authors here): Background
For some individuals, antenatal diagnosis of a congenital heart defect (CHD) allows alternative options to cardiac surgery: pregnancy termination or perinatal hospice care. Understanding drivers of decision-making for these two non-surgical options is critical to guide patient-centered counseling practices. We aimed to explore experiences and decision-making among individuals who chose termination or perinatal hospice care after diagnosis of a fetal CHD.
Methods
This was a qualitative analysis of semi-structured, 1:1 interviews with birthing individuals or their partners from a purposive sample of those who experienced termination or perinatal hospice after receiving multidisciplinary counseling for severe fetal CHD at Lurie Children’s between 2019-2022. The interview guide was comprised of open-ended questions addressing counseling experiences, decision making, and for relevant participants, postnatal experience with perinatal hospice care. The guide was designed by fetal cardiologists, maternal-fetal medicine specialists, neonatologists, palliative care specialists, qualitative researchers, an ethicist, and two parent advisors. Interviews (60-90 minutes) were professionally transcribed and analyzed using Dedoose software. Thematic analysis was conducted with an inductive approach.
Results
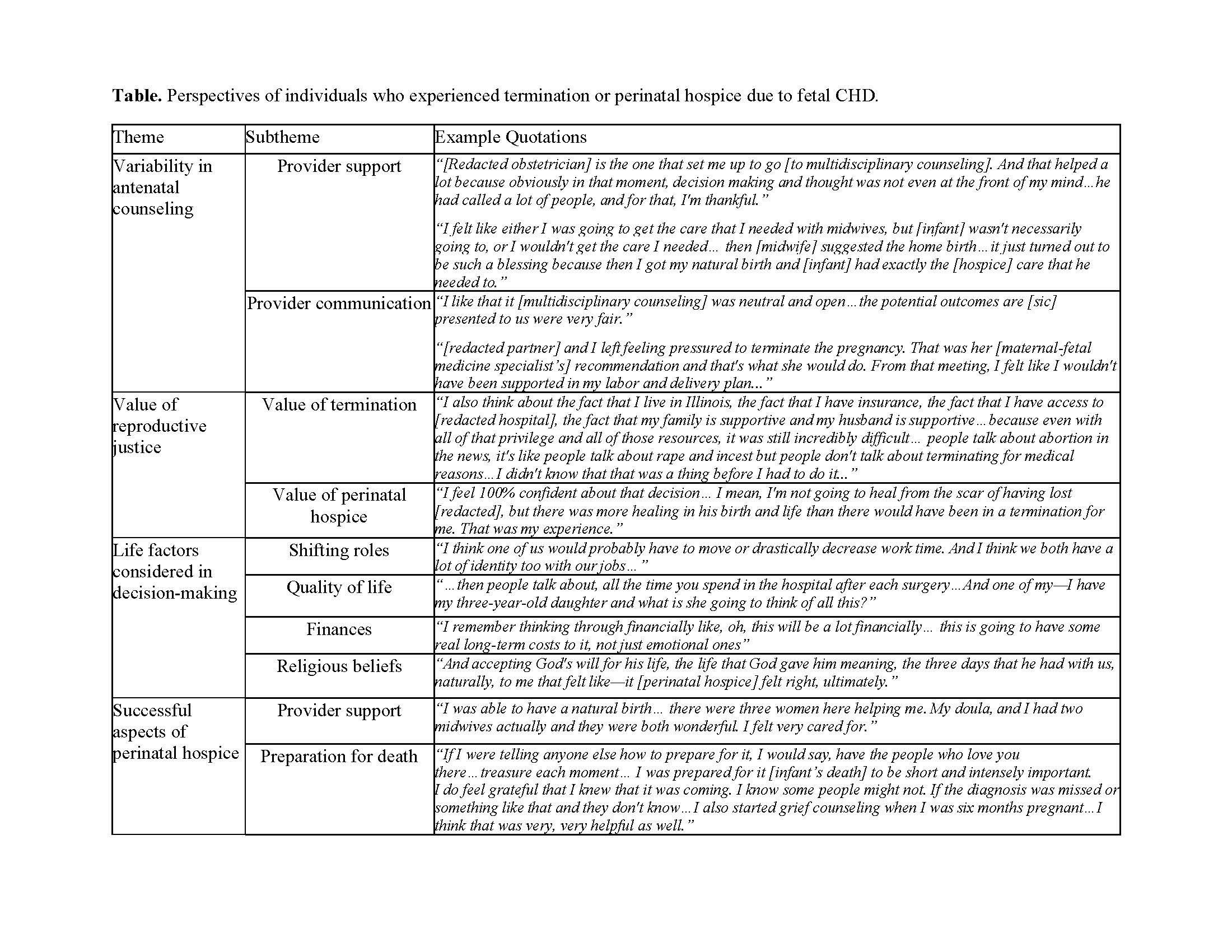
In total, 20 pregnant individuals and their partners met inclusion criteria and were asked to participate. Of these, 10 completed interviews, 9 carried fetuses with single ventricle disease, 2 experienced perinatal hospice care, and 8 identified as non-Hispanic White ethnicity/race. Themes included variability in antenatal counseling, value for reproductive justice, life factors considered in decision-making, and successful aspects of perinatal hospice (Table).
Conclusion
Among individuals who experienced termination or perinatal hospice due to fetal CHD, there is significant variability in the experiences with counseling. Yet, there is shared value for provider support, consideration for life factors in decision-making, and reproductive autonomy. Understanding both the variability and shared themes is key to optimize and standardize counseling practices for fetal CHD.
For some individuals, antenatal diagnosis of a congenital heart defect (CHD) allows alternative options to cardiac surgery: pregnancy termination or perinatal hospice care. Understanding drivers of decision-making for these two non-surgical options is critical to guide patient-centered counseling practices. We aimed to explore experiences and decision-making among individuals who chose termination or perinatal hospice care after diagnosis of a fetal CHD.
Methods
This was a qualitative analysis of semi-structured, 1:1 interviews with birthing individuals or their partners from a purposive sample of those who experienced termination or perinatal hospice after receiving multidisciplinary counseling for severe fetal CHD at Lurie Children’s between 2019-2022. The interview guide was comprised of open-ended questions addressing counseling experiences, decision making, and for relevant participants, postnatal experience with perinatal hospice care. The guide was designed by fetal cardiologists, maternal-fetal medicine specialists, neonatologists, palliative care specialists, qualitative researchers, an ethicist, and two parent advisors. Interviews (60-90 minutes) were professionally transcribed and analyzed using Dedoose software. Thematic analysis was conducted with an inductive approach.
Results
In total, 20 pregnant individuals and their partners met inclusion criteria and were asked to participate. Of these, 10 completed interviews, 9 carried fetuses with single ventricle disease, 2 experienced perinatal hospice care, and 8 identified as non-Hispanic White ethnicity/race. Themes included variability in antenatal counseling, value for reproductive justice, life factors considered in decision-making, and successful aspects of perinatal hospice (Table).
Conclusion
Among individuals who experienced termination or perinatal hospice due to fetal CHD, there is significant variability in the experiences with counseling. Yet, there is shared value for provider support, consideration for life factors in decision-making, and reproductive autonomy. Understanding both the variability and shared themes is key to optimize and standardize counseling practices for fetal CHD.
More abstracts on this topic:
A Shocking Postpartum Course
Wozniak Phillip, Grodzinsky Anna
Aberrant Regulation of endMT in Turner Syndrome: Implications for the Pathogenesis of Congenital Cardiovascular DiseaseGarcia Huitron Eric Ivan, Zhang Xiaoying, Babcock Lance, Grande-allen Kathryn, Prakash Siddharth