Final ID: MDP118
Efficacy of Inferior Vena Cava-Pulmonary Artery Bypass for Right Ventricular Dysfunction under Left Ventricular Assist Device Support: An in vitro study using a biventricular circulation system
Abstract Body (Do not enter title and authors here): Introduction: Right heart failure under the support of a left ventricular assist device (LVAD) presents a life-threatening condition characterized by organ edema and limited LVAD support. Implementing an inferior vena cava-pulmonary artery (IVC-PA) bypass graft may mitigate these complications by reducing central venous pressure (CVP) and improving LVAD support efficiency. This study aimed to elucidate an adequate graft diameter for an IVC-PA bypass in terms of CVP reduction during LVAD-assisted circulation using an in vitro biventricular pulsatile circulatory system.
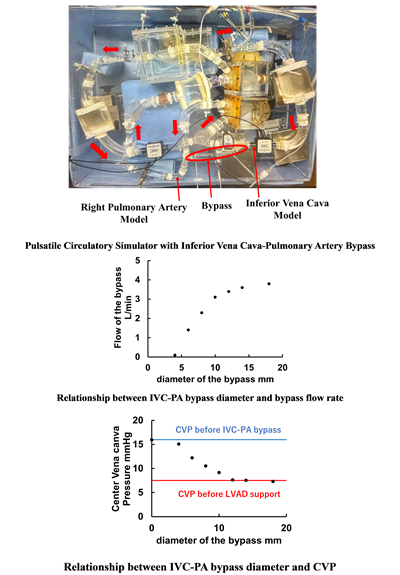
Methods: We developed a biventricular pulsatile circulation system capable of providing circulatory assistance via an LVAD (centrifugal pump) connected to the apex of a left ventricular model (Fig). A representative condition of cardiogenic shock was produced by adjusting LV systolic pressure, aortic pressure, and CVP to 80 mmHg, 80/40 mmHg, and 7.5 mmHg, respectively. A right heart failure model was produced by adjusting LV systolic pressure, aortic pressure, and CVP to 45 mmHg, 70 mmHg, and 16 mmHg, respectively, under LVAD support at 1700 rpm. Then, an adequate IVC-PA bypass diameter was investigated in terms of reducing CVP and increasing bypass flow support among 4mm and 18 mm with 2mm interval. The diameters of PA and IVC, and systolic PA pressure were set to 19 mm, 19 mm, and 18 mmHg, respectively. Elastic LV and RV models were driven by pneumatic positive and negative pressures.
Results: We found a linearly increasing trend of bypass flow and a decreasing trend of CVP with increasing bypass diameters from 4 to 12 mm. When applying the bypass graft over 12mm diameter, bypass flow and CVP plateaued at 3.4 L/min and 7.5 mmHg, respectively (Fig).
Conclusion: Our sophisticated in vitro biventricular circulation study suggests that in scenarios of right heart failure under LVAD support, implementing a bypass graft from the IVC to the PA is effective for decreasing CVP and reducing right ventricular preload. This study indicates that the optimal bypass diameter for reducing CVP is 12 mm when the diameters of the IVC and PA are 19 mm. These findings encouraged us to evaluate the efficacy in in vivo clinical settings.
Methods: We developed a biventricular pulsatile circulation system capable of providing circulatory assistance via an LVAD (centrifugal pump) connected to the apex of a left ventricular model (Fig). A representative condition of cardiogenic shock was produced by adjusting LV systolic pressure, aortic pressure, and CVP to 80 mmHg, 80/40 mmHg, and 7.5 mmHg, respectively. A right heart failure model was produced by adjusting LV systolic pressure, aortic pressure, and CVP to 45 mmHg, 70 mmHg, and 16 mmHg, respectively, under LVAD support at 1700 rpm. Then, an adequate IVC-PA bypass diameter was investigated in terms of reducing CVP and increasing bypass flow support among 4mm and 18 mm with 2mm interval. The diameters of PA and IVC, and systolic PA pressure were set to 19 mm, 19 mm, and 18 mmHg, respectively. Elastic LV and RV models were driven by pneumatic positive and negative pressures.
Results: We found a linearly increasing trend of bypass flow and a decreasing trend of CVP with increasing bypass diameters from 4 to 12 mm. When applying the bypass graft over 12mm diameter, bypass flow and CVP plateaued at 3.4 L/min and 7.5 mmHg, respectively (Fig).
Conclusion: Our sophisticated in vitro biventricular circulation study suggests that in scenarios of right heart failure under LVAD support, implementing a bypass graft from the IVC to the PA is effective for decreasing CVP and reducing right ventricular preload. This study indicates that the optimal bypass diameter for reducing CVP is 12 mm when the diameters of the IVC and PA are 19 mm. These findings encouraged us to evaluate the efficacy in in vivo clinical settings.
More abstracts on this topic:
Ascending Thoracic Aortic Aneurysms in a Veterans Affairs Health System: Longitudinal Outcomes and Risk Factors
Gomez Axel, Carroway William, Ge Liang, Boskovski Marko, Tseng Elaine
Anomalous Origin Of Left Circumflex Artery From Right Pulmonary Artery Resulting In Heart Failure: A Rare Vascular Steal PhenomenonChander Yogesh, Bhardwaj Rajeev, Nandal Rajesh, Mittal Saurav, Pruthi Taniya, Singh Subeg