Final ID: Sa3116
Surveying Healthcare Professionals' Awareness and Management of Inflammation as a Residual Cardiovascular Risk Factor.
Methods: The survey, consisting of 20 questions dedicated to HCPs, was developed by the International Lipid Expert Panel (ILEP). It was launched in March 2024 and promoted through websites, SoMe channels, and newsletters. Many questions allowed for multiple responses. The questionnaire is ongoing and available at the ILEP webpage.
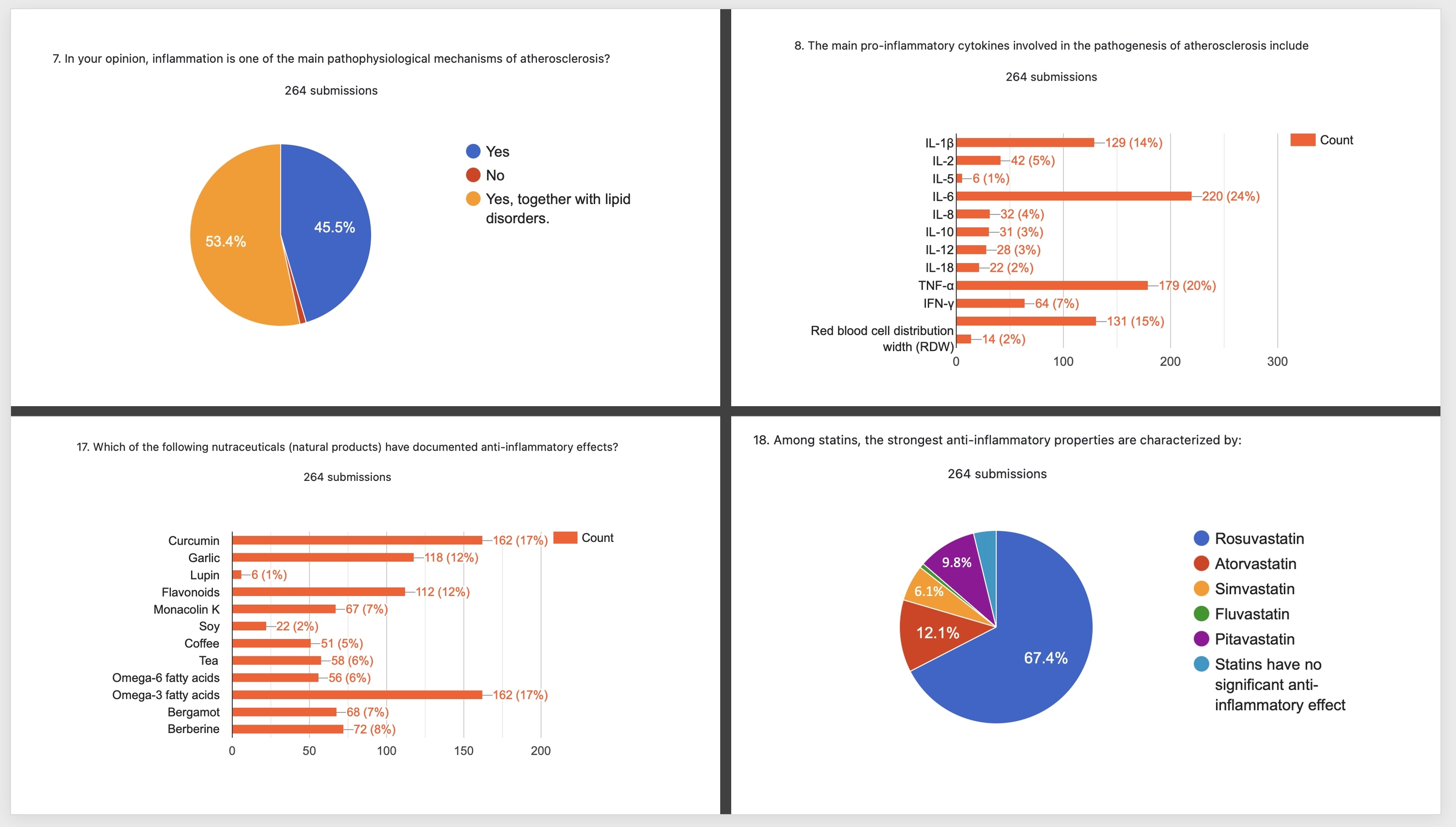
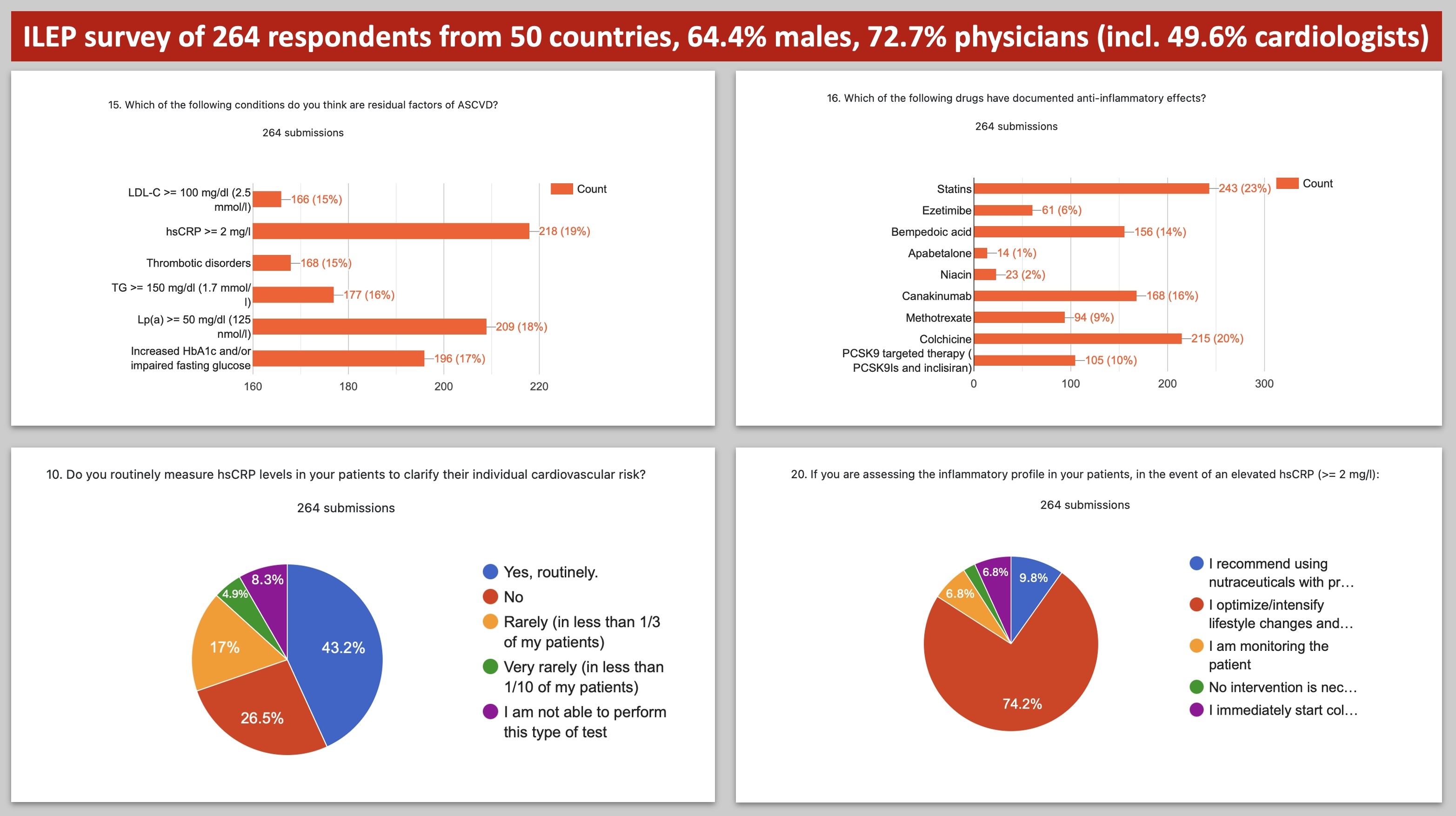
Results: We collected 264 responses within 3 months (64.4% males; 50.8% between 40-59 yrs.), mostly from physicians (72.7%, of which 49.6% were cardiologists, and 16.3% internal medicine specialists), but also researchers (6.8%) and academics (6.4%). HCPs from 50 countries participated in the survey. The highest response rates were from Poland: 26.9%, USA: 17.4%, Greece and Romania (4.5% for both). Only 43.4% of responders routinely measure hsCRP for CVD risk stratification, and only 20% had possibilities to measure both CRP, hsCRP, and IL-6. 28% knew the difference between CRP and hsCRP tests, and only 54.9% knew the approved hsCRP ranges to stratify CVD risk. 47.7% of the respondents recognized CRP as a causal risk factor of CVD, with only every 5th recognizing IL-6 (Fig.1). 71.2% of HCPs accepted statins, colchicine, and bempedoic acid as available therapies that might effectively reduce hsCRP elevated levels (Fig.1&2); 11% suggested that one should only reduce general CVD risk. Besides having rather general knowledge of the anti-inflammatory role of statins or colchicine, there are still 23.1% and 39.8% of responders that recognized anti-inflammatory properties of ezetimibe and PCSK9 modulators, respectively (Fig.2). A lot of inconsistency exists on the knowledge of the potential anti-inflammatory role of natural products, with the highest number of responses indicating curcumin and omega-3 acids (61.4% for both) (Fig.1). In the case of elevated hsCRP, 74.2% of HCPs recommended intensification of lifestyle changes and background CVD therapies, while 9.8% suggested using nutraceuticals, and 6.8% were prone to just monitoring the patients (Fig.2).
Conclusions: There is a significant gap in knowledge regarding the diagnosis, biomarkers, and management of inflammation in CVD risk stratification. Enhanced education for medical students, physicians, and patients is crucial before targeted therapies become widely available.
- Banach, Maciej ( UMED, Lodz, Poland , Lodz , Poland )
- Postadzhiyan, Arman ( University Hospital St. Ana , SOFIA , Bulgaria )
- Moriarty, Patrick ( University of Kansas Medical Center , Kansas City , Missouri , United States )
- Vohnout, Branislav ( Slovak Medical University in Bratislava , Bratislava , Slovakia )
- Jozwiak, Jacek ( University of Opole , Opole , Poland )
- Shapiro, Michael ( Wake Forest Univ School of Medicine , Winston Salem , North Carolina , United States )
- Wong, Nathan ( UNIV OF CALIFORNIA IRVINE , Irvine , California , United States )
- Surma, Stanislaw ( Silesian Medical University , Katowice , Poland )
- Alnouri, Fahad ( Prince Sultan Cardiac Centre Riyadh , Riyadh , Saudi Arabia )
- Mancini, G B John ( University of British Columbia, , Vancouver , British Columbia , Canada )
- Vinereanu, Dragos ( University of Medicine and Pharmacy Carol Davila , Bucharest , Romania )
- Gouni-berthold, Ioanna ( University of Cologne, Department o , Cologne , Germany )
- Reiner, Zeljko ( UNIVERSITY HOSPITAL CENTER ZAGREB , Zagreb , Croatia )
- Sabouret, Pierre ( PITIE SALPETRIERE-HEART INSTITUTE , PARIS , France )
- Latkovskis, Gustavs ( Pauls Stradins Hospital , Riga , Latvia )
Meeting Info:
Session Info:
Medley of Cardiovascular Risk Factors, Stratification, and Prediction
Saturday, 11/16/2024 , 10:30AM - 11:30AM
Abstract Poster Session
More abstracts on this topic:
Abdulkarim Iya, Metzger Joseph, Stovitz Steven, Van't Hof Jeremy
A RETRO-ENANTIOMER OF ANGIOTENSIN-(1-9) PREVENTS THE DEVELOPMENT OF HEART FAILURE WITH PRESERVED EJECTION FRACTION.Ocaranza Maria Paz, Jimenez Veronica, Yanez Osvaldo, Jalil Jorge, Venegas Camilo, Candia Camila, Hermoso Marcela, Gabrielli Luigi, Morales Javier, Oyarzun Felipe, Torres Cristian, Lillo Pablo
More abstracts from these authors:
The Results of the International Survey
Surma Stanislaw, Lewek Joanna, Sobierajski Tomasz, Banach Maciej
Association between Clinical Characteristics and Telomere Length - Factor Analysis of Mixed Data (FAMD)-based Cluster AnalysisOsadnik Tadeusz, Gierlotka Marek, Golawski Marcin, Osadnik Kamila, Fronczek Martyna, Gach Agnieszka, Jozwiak Jacek, Banach Maciej, Goc Anna, Boniewska-bernacka Ewa, Panczyszyn Anna, Lejawa Mateusz, Strzelczyk Joanna, Pawlas Natalia, Krystek Karol