Final ID: Su2045
Incidence of Autoimmune Disease in Hospitalized Patients with Congenital Heart Disease
Abstract Body (Do not enter title and authors here): Introduction
Individuals with congenital heart disease (CHD) have increased risk of immune suppression and elevated inflammatory markers in response to abnormal cardiac physiology. This pathologic milieu may put them at risk for developing autoimmune disease (AID).
Hypothesis
We hypothesized a higher incidence of AID in patients with CHD.
Methods
We conducted a retrospective review of the Vizient® Clinical Data Base (a national, administrative database) from 10/2019–12/2023 for admissions aged 1-25 years with ICD-10 codes for AID, with and without ICD-10 codes for CHD. ICD-10 codes for 22q11 deletion were also included in the query due to its potential confounding immunologic effects. Data included: demographics, length of stay (LOS), complication and in-hospital mortality rates, and costs. Comparisons were made between the groups with CHD and AID and those without AID (NO-AID).
Results
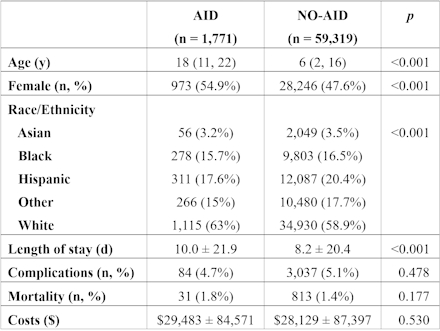
There were 4,680,247 admissions without 22q11 deletion. Of these admissions, there was a lower incidence of AID in the CHD group compared to those without CHD [1,771 (0.7%) vs 59319 (1.3%), p<0.001]. There was no difference in 22q11 deletion in CHD admissions with AID and those without (2.1 vs 2.2%, p=0.643); only the population without 22q11 deletion was analyzed further. Of 61,090 admissions with CHD, there were 1,771 with AID and 59,319 with NO-AID. Details are in Table 1. CHD patients with AID were older (18 vs 6 years), more likely female (54.9% vs 47.6%), more commonly White individuals (63% vs 58.9%) and had longer LOS (p<0.001 for all). There were no differences in complication and mortality rates or costs.
Conclusions
This national database review suggests a lower incidence of AID in patients with CHD compared to those without CHD. However, patients with CHD and AID were older and had a longer LOS. These findings highlight a possible time-dependent component in AID development, as well the potential negative effects on hospital outcomes in the setting of multiple, complex comorbid conditions.
Individuals with congenital heart disease (CHD) have increased risk of immune suppression and elevated inflammatory markers in response to abnormal cardiac physiology. This pathologic milieu may put them at risk for developing autoimmune disease (AID).
Hypothesis
We hypothesized a higher incidence of AID in patients with CHD.
Methods
We conducted a retrospective review of the Vizient® Clinical Data Base (a national, administrative database) from 10/2019–12/2023 for admissions aged 1-25 years with ICD-10 codes for AID, with and without ICD-10 codes for CHD. ICD-10 codes for 22q11 deletion were also included in the query due to its potential confounding immunologic effects. Data included: demographics, length of stay (LOS), complication and in-hospital mortality rates, and costs. Comparisons were made between the groups with CHD and AID and those without AID (NO-AID).
Results
There were 4,680,247 admissions without 22q11 deletion. Of these admissions, there was a lower incidence of AID in the CHD group compared to those without CHD [1,771 (0.7%) vs 59319 (1.3%), p<0.001]. There was no difference in 22q11 deletion in CHD admissions with AID and those without (2.1 vs 2.2%, p=0.643); only the population without 22q11 deletion was analyzed further. Of 61,090 admissions with CHD, there were 1,771 with AID and 59,319 with NO-AID. Details are in Table 1. CHD patients with AID were older (18 vs 6 years), more likely female (54.9% vs 47.6%), more commonly White individuals (63% vs 58.9%) and had longer LOS (p<0.001 for all). There were no differences in complication and mortality rates or costs.
Conclusions
This national database review suggests a lower incidence of AID in patients with CHD compared to those without CHD. However, patients with CHD and AID were older and had a longer LOS. These findings highlight a possible time-dependent component in AID development, as well the potential negative effects on hospital outcomes in the setting of multiple, complex comorbid conditions.
More abstracts on this topic:
β1 integrins regulate cellular behavior and cardiomyocyte organization during ventricular wall formation
Miao Lianjie, Schwartz Robert, R Burns Alan, Kumar Ashok, Dipersio C. Michael, Wu Mingfu, Lu Yangyang, Nusrat Anika, Zhao Luqi, Castillo Micah, Xiao Yongqi, Guo Hongyan, Liu Yu, Gunaratne Preethi
A Rare Manifestation of Drug-Induced Lupus: Hydralazine-Induced ANCA Vasculitis and Persistent PericarditisSaini Ishveen, Vo Phuong Uyen, Slabic Andrew, Varian Kenneth