Final ID: Sa2009
Immunologic Insights: Activated and Exhausted Circulating T-Cell Phenotype in Hypoplastic Left Heart Syndrome (HLHS)
Abstract Body (Do not enter title and authors here): Background. While staged surgical palliation for infants born with hypoplastic left heart syndrome (HLHS) has enabled many patients to survive a previously fatal condition, there is now a growing population of HLHS children and young adults who experience significant co-morbidities and mortality secondary to their palliated physiology. Abnormalities of the immune system, including T-cell lymphopenia, have been documented in HLHS patients. However, the impact of altered T-cell homeostasis remains ill-defined.
Hypothesis. Both intrinsic and acquired alterations in T-cell sub-populations results in T-cell activation/exhaustion and a pro-inflammatory phenotype.
Methods. Peripheral T-cell sub-populations and activation/inhibition markers were quantified in HLHS (n=32, median age 1.65 years, range 0-13.2 years) and healthy, pediatric controls (n=14, median age 4.55 years, range 0.2-15.1 years) by mass cytometry (Helios Cytometry Time Of Flight, CyTOF). Comparison between HLHS and controls was performed by unpaired t-test or Mann-Whitney, based on normality.
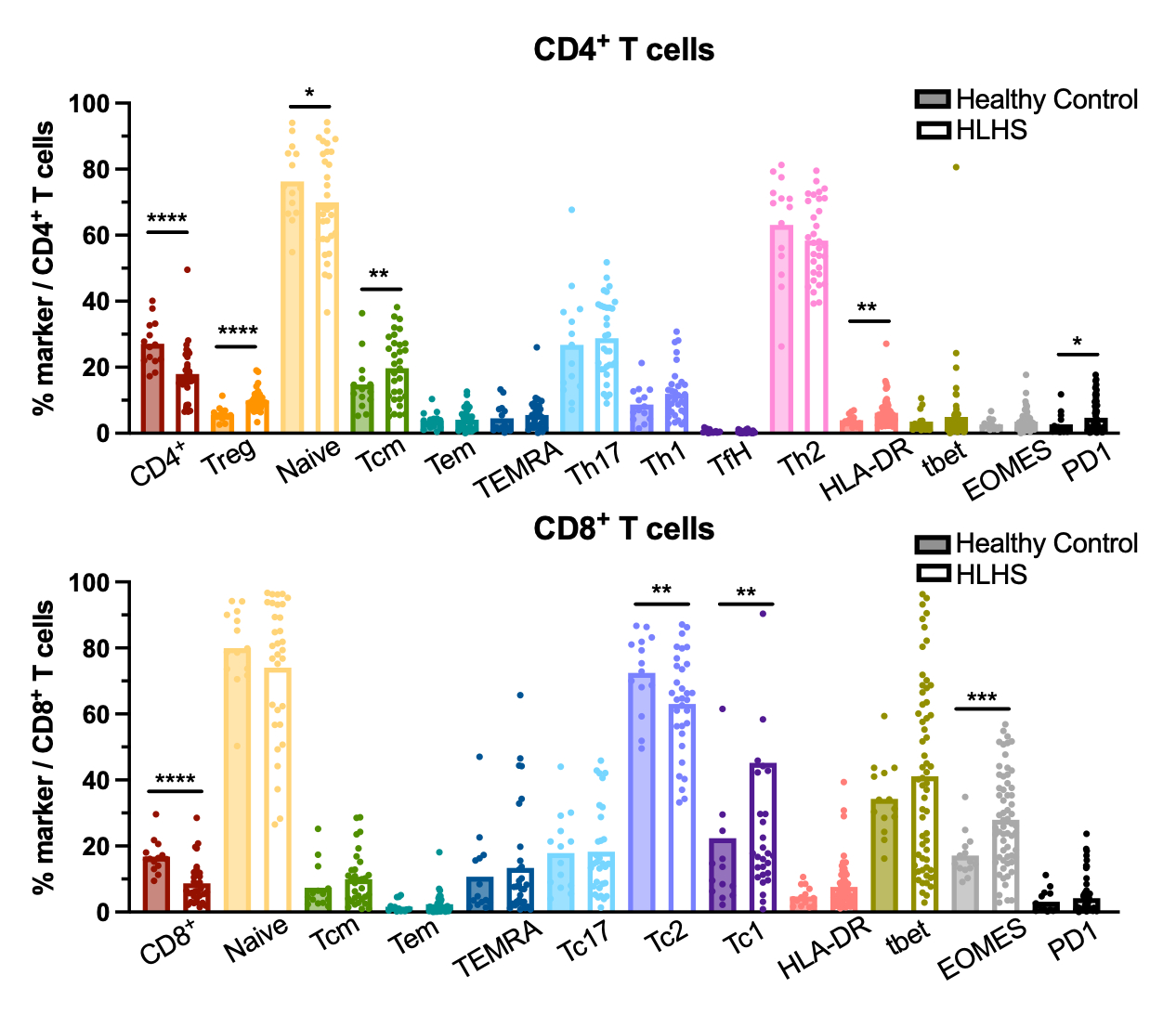
Results. In HLHS subjects, circulating CD4+ and CD8+ populations are significantly decreased (p<0.001) compared to control. The proportions of CD4+HLA-DR+ (p<0.05) and CD8+EOMES+ (p<0.01) T cells are increased in HLHS. HLHS CD8+TC1+ populations are increased (p<0.05) while HLHS CD8+TC2+ (p<0.05) populations are decreased compared to controls. Notably, there is an increase in CD4+ regulatory T cells in HLHS subjects (p<0.001).
Conclusions. Immunoprofiling of peripheral T-cell populations suggests that abnormalities extend beyond a decrease in T-cell numbers: HLHS T cells demonstrate an activated and exhausted phenotype, which may impact development of co-morbidities in this population. Additional investigations are required to delineate the functional consequences of this unique HLHS immunophenotype.
Hypothesis. Both intrinsic and acquired alterations in T-cell sub-populations results in T-cell activation/exhaustion and a pro-inflammatory phenotype.
Methods. Peripheral T-cell sub-populations and activation/inhibition markers were quantified in HLHS (n=32, median age 1.65 years, range 0-13.2 years) and healthy, pediatric controls (n=14, median age 4.55 years, range 0.2-15.1 years) by mass cytometry (Helios Cytometry Time Of Flight, CyTOF). Comparison between HLHS and controls was performed by unpaired t-test or Mann-Whitney, based on normality.
Results. In HLHS subjects, circulating CD4+ and CD8+ populations are significantly decreased (p<0.001) compared to control. The proportions of CD4+HLA-DR+ (p<0.05) and CD8+EOMES+ (p<0.01) T cells are increased in HLHS. HLHS CD8+TC1+ populations are increased (p<0.05) while HLHS CD8+TC2+ (p<0.05) populations are decreased compared to controls. Notably, there is an increase in CD4+ regulatory T cells in HLHS subjects (p<0.001).
Conclusions. Immunoprofiling of peripheral T-cell populations suggests that abnormalities extend beyond a decrease in T-cell numbers: HLHS T cells demonstrate an activated and exhausted phenotype, which may impact development of co-morbidities in this population. Additional investigations are required to delineate the functional consequences of this unique HLHS immunophenotype.
More abstracts on this topic:
Cardiac magnetic resonance imaging findings and their association with exercise performance – data from the Single Ventricle Reconstruction Trial longitudinal follow-up
Detterich Jon, Prospero Carol, Cartoski Mark, Binka Edem, Vaiyani Danish, Lang Sean, Trachtenberg Felicia, Newburger Jane, Goldberg Caren, Taylor Michael, Dorfman Adam, Slesnick Timothy, Shah Amee, Nutting Arni, Seed Mike, Campbell Michael, Goot Ben, Prakash Ashwin
Decoding Endocardial Fibroelastosis with Differentially Regulated miR-100-5p and miR-503-5pZajac Cindy, Del Nido Pedro, Friehs Ingeborg, Gaal Julia, Costa De Freitas Renata Caroline, Diaz-gil Daniel, Zhu Yonglin, Saraci Kerstin, Gierlinger Gregor, Melero-martin Juan, Axt-fliedner Roland