Final ID: Su3180
Disparities in Healthcare Utilization following Endovascular Abdominal Aneurysm Repair
Abstract Body (Do not enter title and authors here): Introduction: Healthcare utilization in postoperative management and surveillance following endovascular aneurysm repair (EVAR) is an important factor in achieving long-term treatment success. However, factors associated with poor healthcare utilization have yet to be elucidated.
Hypothesis: Disadvantaged patients have lower rates of surveillance and higher rates of emergency health service use than their counterparts.
Aims: Examine rates of healthcare utilization stratified by age, sex, race, dual-enrollment in Medicare and Medicaid, and residence in a distressed community.
Methods: We performed an observational retrospective cohort study of Medicare beneficiaries who underwent infrarenal EVAR with a bifurcated endograft between 2011-2019. We examined annual rates of post-operative surveillance (EVAR-related outpatient visits, surveillance imaging), use of emergency department (ED) visits, and hospital readmission across several disparity measures using Modified Poisson Regression models.
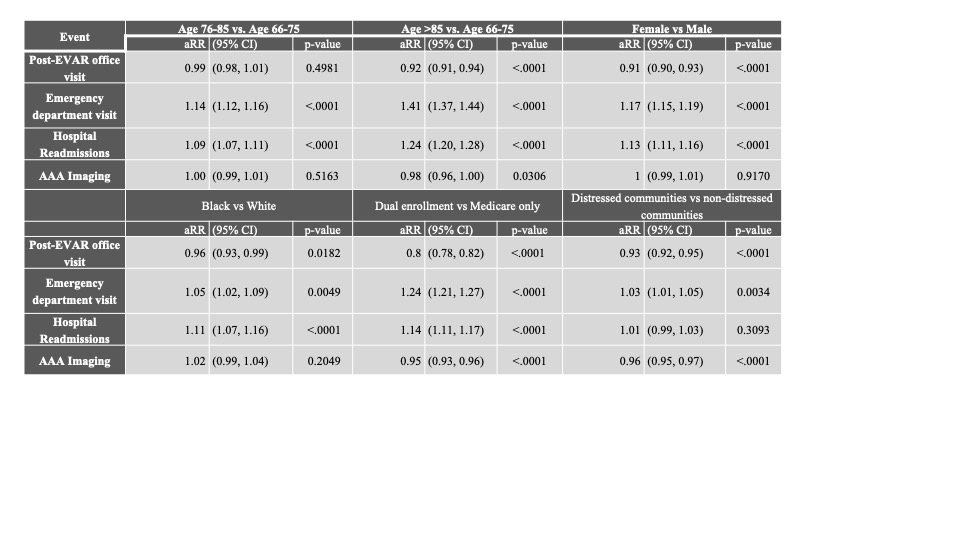
Results: In 111,381 Medicare beneficiaries undergoing EVAR, comorbidities associated with poor postoperative surveillance were chronic kidney disease (aRR:1.06[1.04-1.07]), heart failure (1.10[1.09-1.11]), hyperlipidemia (1.16[1.14-1.19]), hypertension (1.09[1.07-1.12]), and ischemic heart disease (1.15[1.14-1.17]). For EVAR-related office visits, patients with worse post-operative care included those >85 years, female, Black, dual-enrolled, or living in distressed communities (Table 1). Similarly, less surveillance imaging was performed in patients >85 years, dual-enrolled, or living in distressed communities. There was a greater need for ER care or readmission among patients >85 years, female, Black, dual-enrolled, or living in distressed communities.
Conclusions: Our study revealed patterns of disparities in post-procedure EVAR-related office visits and EVAR imaging studies, and greater use of emergency health services associated with patient age, sex, race, and socioeconomic status. These findings may suggest barriers in access to appropriate surveillance and care which could be addressed by targeting the identified groups for intervention efforts to improve EVAR surveillance.
Hypothesis: Disadvantaged patients have lower rates of surveillance and higher rates of emergency health service use than their counterparts.
Aims: Examine rates of healthcare utilization stratified by age, sex, race, dual-enrollment in Medicare and Medicaid, and residence in a distressed community.
Methods: We performed an observational retrospective cohort study of Medicare beneficiaries who underwent infrarenal EVAR with a bifurcated endograft between 2011-2019. We examined annual rates of post-operative surveillance (EVAR-related outpatient visits, surveillance imaging), use of emergency department (ED) visits, and hospital readmission across several disparity measures using Modified Poisson Regression models.
Results: In 111,381 Medicare beneficiaries undergoing EVAR, comorbidities associated with poor postoperative surveillance were chronic kidney disease (aRR:1.06[1.04-1.07]), heart failure (1.10[1.09-1.11]), hyperlipidemia (1.16[1.14-1.19]), hypertension (1.09[1.07-1.12]), and ischemic heart disease (1.15[1.14-1.17]). For EVAR-related office visits, patients with worse post-operative care included those >85 years, female, Black, dual-enrolled, or living in distressed communities (Table 1). Similarly, less surveillance imaging was performed in patients >85 years, dual-enrolled, or living in distressed communities. There was a greater need for ER care or readmission among patients >85 years, female, Black, dual-enrolled, or living in distressed communities.
Conclusions: Our study revealed patterns of disparities in post-procedure EVAR-related office visits and EVAR imaging studies, and greater use of emergency health services associated with patient age, sex, race, and socioeconomic status. These findings may suggest barriers in access to appropriate surveillance and care which could be addressed by targeting the identified groups for intervention efforts to improve EVAR surveillance.
More abstracts on this topic:
Adaptive Cardiac Arrest Training Curriculum for Capacity Building in Northern Ghana: Addressing Contextual Challenges for Sustainability
Ahadzi Dzifa, Boateng Laud, Hernandez Odalys Rivera, Akanbong Prosper, Leung Claudia, Al-hassan Rahma, Baba Yabasin Iddrisu, Yakubu Abdul-subulr, Cournooh Annette, Ikeda Scott, Alomatu Samuel, Sakeah Patience
Active Screening in Black, Hispanic/LatinX, Asian/Pacific Islander, and Native American Individuals Reduces Racial Disparities in Abdominal Aortic Aneurysm DiagnosisMiner Grace, Govindarajulu Usha, Smolock Christopher, Faries Peter, Marin Michael