Final ID: MDP1004
Heart Failure Quality of Care and Outcomes among Asian Ethnic Groups in the United States
Abstract Body (Do not enter title and authors here): Background: Asian populations in the United States experience heterogenous burden of cardiovascular disease (CVD). Heart failure (HF) hospitalization quality of care or outcomes have not been reported in these populations.
Methods: Participants were adults age ≥18 years in the AHA Get with the Guidelines Heart Failure registry (2015-2023) who had a primary admission diagnosis of HF, and identified as Asian Indian, Chinese, Filipino, Japanese, Korean, and Vietnamese, or non-Hispanic White (NHW). Odds of optimal medical therapy (receiving up to three medication classes for which they were eligible based on ejection fraction [EF] and absence of contraindication [1: ACE inhibitor, ARB, or ARNI; 2: beta blocker; 3: mineralocorticoid receptor antagonist]), length of stay >4 days, and in-hospital mortality were evaluated in each Asian subgroup vs. NHW, with sex-stratified multivariable logistic regression models, adjusted for age; EF; diabetes, hypertension, and smoking history; and insurance status.
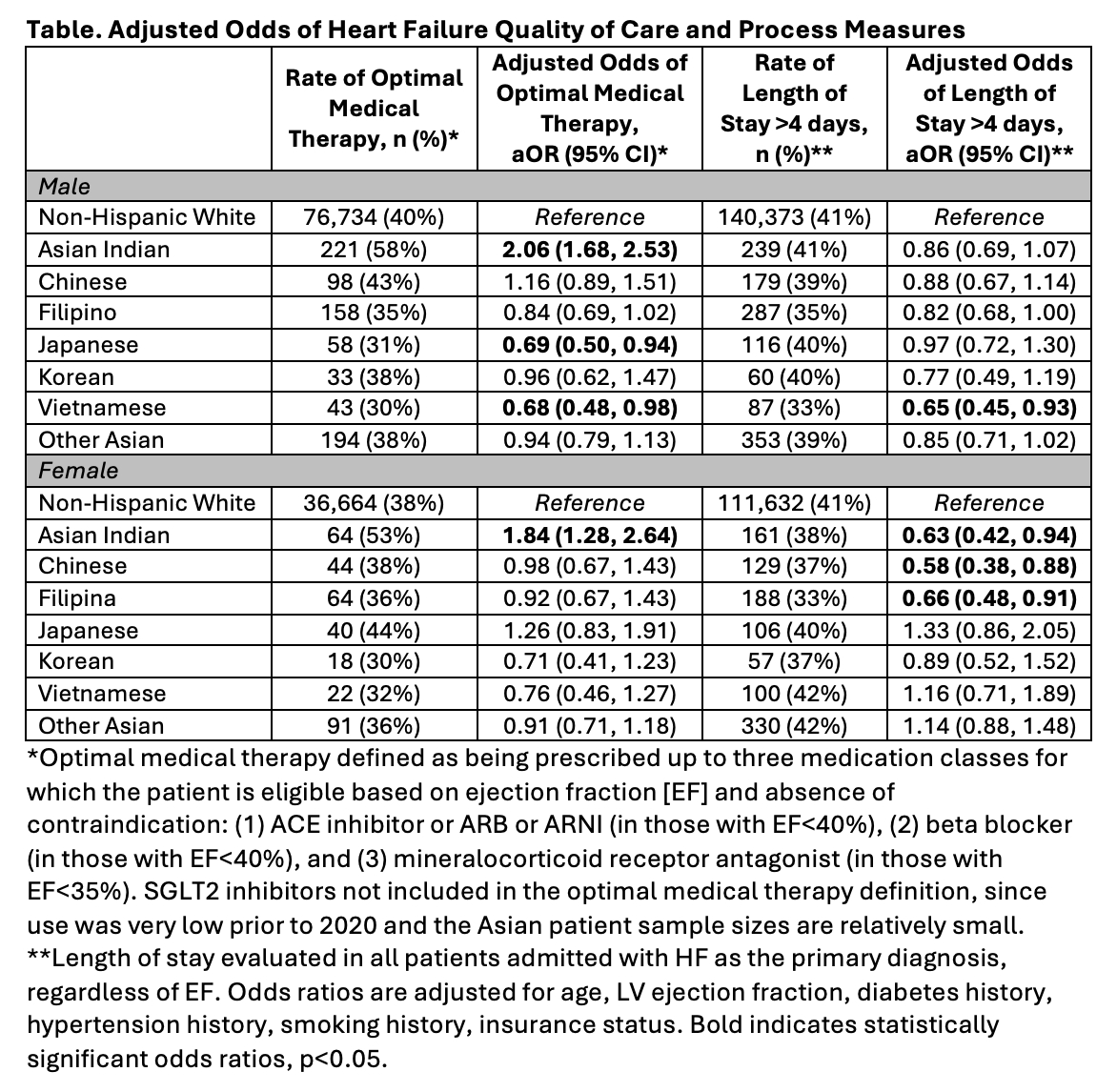
Results: Among Asian (n=3,112) and NHW (n=315,994) registry patients with HF and reduced EF<40%, adjusted odds of optimal medical therapy vs. NHW were lower in Japanese (adjusted odds ratio [aOR] 0.69, 95% confidence interval [CI] 0.50, 0.94) and Vietnamese (aOR 0.68, 95% CI 0.48, 0.98) male patients, and higher in Asian Indian patients (male aOR 2.06, 95% CI 1.68, 2.53; female aOR 1.84, 95% CI 1.28, 2.64) (Table). Among Asian (n=7,261) and NHW (n=790,237) registry patients with HF and any EF, likelihood of length of stay >4 days vs. NHW was lower in Vietnamese male (aOR 0.65, 95% CI 0.45, 0.93), and Asian Indian (aOR 0.63, 95% CI 0.42, 0.94), Chinese (aOR 0.58, 95% CI 0.38, 0.88), and Filipina (aOR 0.66, 95% CI 0.48, 0.91) female patients. In-hospital mortality occurred in 2-4% of Asian patients and 3% of NHW patients, with no statistically significant differences in in-hospital mortality rates in Asian compared with NHW patients.
Conclusions: HF quality of care may vary among Asian subgroups in the US. Quality improvement programs must identify and address the factors that result in variations in HF care among US Asian patients.
Methods: Participants were adults age ≥18 years in the AHA Get with the Guidelines Heart Failure registry (2015-2023) who had a primary admission diagnosis of HF, and identified as Asian Indian, Chinese, Filipino, Japanese, Korean, and Vietnamese, or non-Hispanic White (NHW). Odds of optimal medical therapy (receiving up to three medication classes for which they were eligible based on ejection fraction [EF] and absence of contraindication [1: ACE inhibitor, ARB, or ARNI; 2: beta blocker; 3: mineralocorticoid receptor antagonist]), length of stay >4 days, and in-hospital mortality were evaluated in each Asian subgroup vs. NHW, with sex-stratified multivariable logistic regression models, adjusted for age; EF; diabetes, hypertension, and smoking history; and insurance status.
Results: Among Asian (n=3,112) and NHW (n=315,994) registry patients with HF and reduced EF<40%, adjusted odds of optimal medical therapy vs. NHW were lower in Japanese (adjusted odds ratio [aOR] 0.69, 95% confidence interval [CI] 0.50, 0.94) and Vietnamese (aOR 0.68, 95% CI 0.48, 0.98) male patients, and higher in Asian Indian patients (male aOR 2.06, 95% CI 1.68, 2.53; female aOR 1.84, 95% CI 1.28, 2.64) (Table). Among Asian (n=7,261) and NHW (n=790,237) registry patients with HF and any EF, likelihood of length of stay >4 days vs. NHW was lower in Vietnamese male (aOR 0.65, 95% CI 0.45, 0.93), and Asian Indian (aOR 0.63, 95% CI 0.42, 0.94), Chinese (aOR 0.58, 95% CI 0.38, 0.88), and Filipina (aOR 0.66, 95% CI 0.48, 0.91) female patients. In-hospital mortality occurred in 2-4% of Asian patients and 3% of NHW patients, with no statistically significant differences in in-hospital mortality rates in Asian compared with NHW patients.
Conclusions: HF quality of care may vary among Asian subgroups in the US. Quality improvement programs must identify and address the factors that result in variations in HF care among US Asian patients.
More abstracts on this topic:
A Cardiac Targeting Peptide Linked to miRNA106a Targets and Suppresses Genes Known to Cause Heart Failure: Reversing Heart Failure at the Source
Lu Ming, Deng Claire, Taskintuna Kaan, Ahern Gerard, Yurko Ray, Islam Kazi, Zahid Maliha, Gallicano Ian
Active Screening in Black, Hispanic/LatinX, Asian/Pacific Islander, and Native American Individuals Reduces Racial Disparities in Abdominal Aortic Aneurysm DiagnosisMiner Grace, Govindarajulu Usha, Smolock Christopher, Faries Peter, Marin Michael