Final ID: MDP1194
Blood Pressure in Adolescence and Stroke at a Young Age in 1.9 Million Males and Females
Methods: A nationwide, population-based, retrospective cohort study including data of all Israeli adolescents (16-19 years) who were evaluated prior to mandatory military service in 1985 through 2013. The medical evaluation included routine measurements of height, weight, and blood pressure. The primary outcome was the first occurrence of a stroke at a young age (≤52 years) as documented in the National Stroke Registry. Cox proportional hazard models were applied separately for males and females and adjusted for adolescent body mass index and sociodemographic variables. Diabetes status in adulthood, as documented in the National Diabetes Registry, was also accounted. Several sensitivity analyses were conducted, including the evaluation of ischemic stroke cases only as the outcome and stroke occurrence at a very young age (≤45 years).
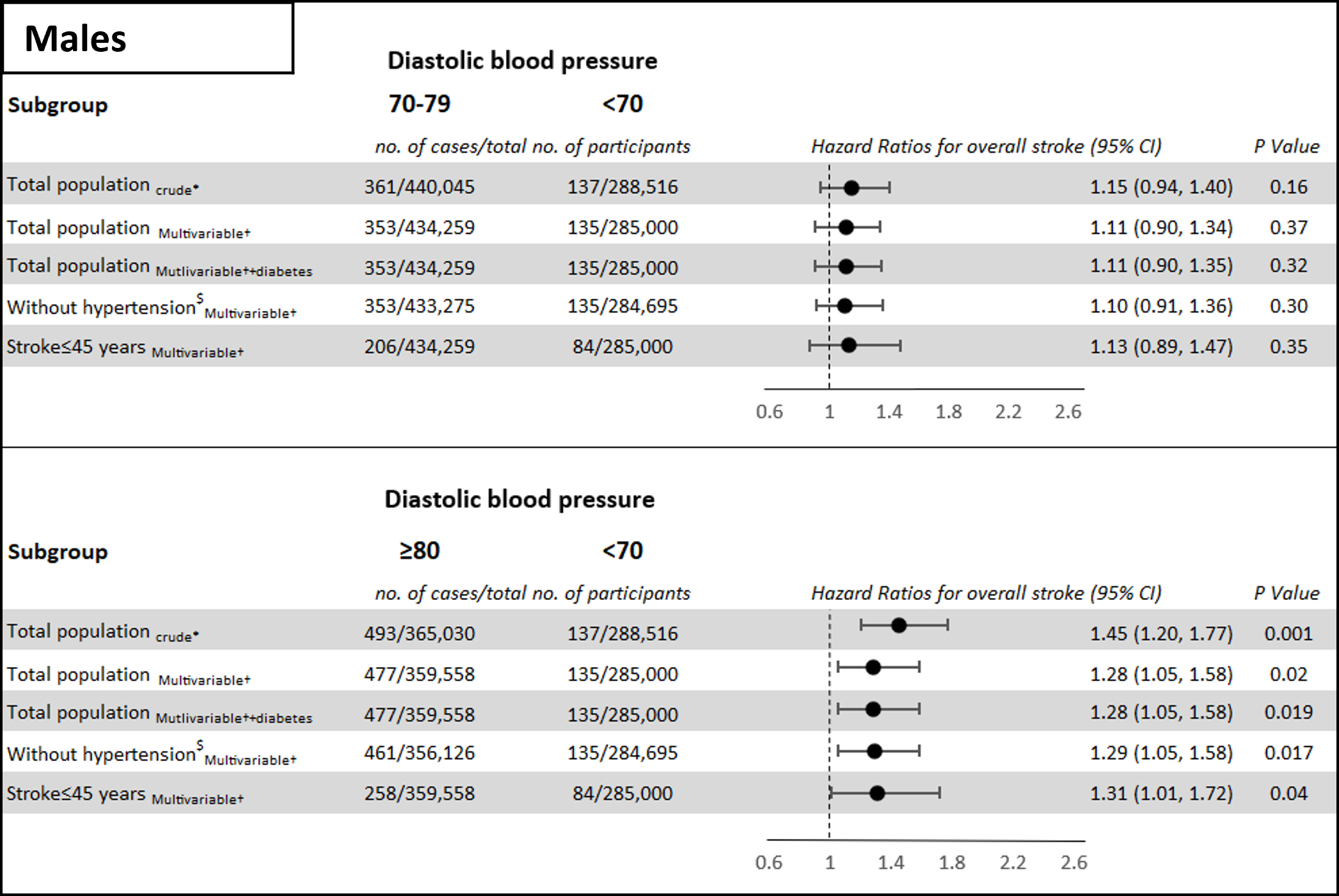
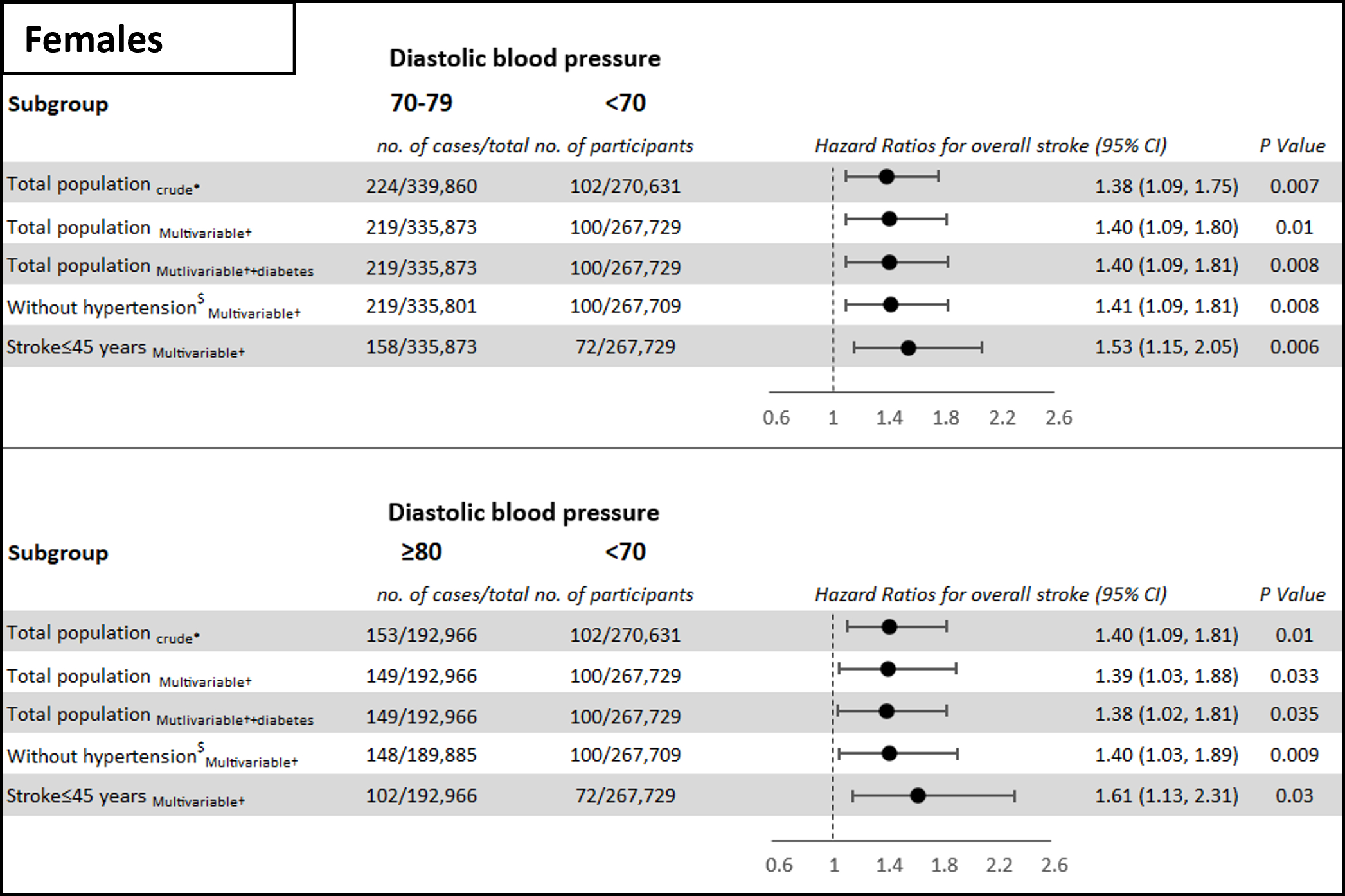
Results: The cohort comprised 1,897,048 adolescents (42.4% females). During 11,355,476 person-years of follow-up, there were 1,470 first stroke events, 1,233 (83.8%) cases were of ischemic etiology. In male adolescents, a diastolic blood pressure of ≥80 mmHg was associated with an adjusted hazard ratio (aHR) for stroke at a young age of 1.28 (95% confidence interval 1.05-1.58) (Image 1). In male adolescents with blood pressure of 70-79 mmHg, the aHR was comparable to that of the reference group (<70 mmHg). The aHRs of female adolescents with a blood pressure of 70-79 mmHg and ≥80 mmHg were 1.40 (1.09-1.80) and 1.39 (1.03-1.88), respectively (Image 2). In the sub-analysis of ischemic stroke cases as the outcome, the aHRs were 1.63 (1.23-2.16) and 1.59 (1.14-2.22) for females with blood pressure of 70-79 mmHg and ≥80 mmHg, respectively. The results persisted in extensive sensitivity analysis (Image 1, Image 2).
Adolescent systolic blood pressure of 120-129 mmHg or ≥130 mmHg compared to <120 mmHg was not associated with the outcome in adolescents of both sexes.
Conclusions: Diastolic blood pressure in adolescence was associated with stroke at a young age, with a lower cutoff level among females.
- Coresh, Josef ( NYU Grossman School of Medicine , New York , New York , United States )
- Ram, Amit ( MOH , Ramat Gan , Israel )
- Hershkovitz, Yael ( MOH , Ramat Gan , Israel )
- Orr, Omri ( Rambam Health Care Campus , Haifa , Israel )
- Furer, Ariel ( Hebrew University , Jerusalem , Israel )
- Perelman, Maxim ( Hebrew University , Jerusalem , Israel )
- Chodick, Gabriel ( Tel Aviv University , Ramat Gan , Israel )
- Yaniv, Gal ( Sheba Medical Center , Ramat Gan , Israel )
- Tanne, David ( Rambam Health Care Campus , Haifa , Israel )
- Derazne, Estela ( Tel Aviv University , Ramat Gan , Israel )
- Tzur, Dorit ( Hebrew University , Jerusalem , Israel )
- Fishman, Boris ( UPMC , Pittsburgh , Pennsylvania , United States )
- Afek, Arnon ( Sheba Medical Center , Ramat Gan , Israel )
- Grossman, Ehud ( CHAIM SHEBA MEDICAL CTR , Tel Hashomer , Israel )
- Twig, Gilad ( Sheba Medical Center , Ramat Gan , Israel )
- Vinograd, Adi ( MOH , Ramat Gan , Israel )
- Tsur, Avishai M ( Tel Aviv University , Ramat Gan , Israel )
- Bardugo, Aya ( Hebrew University , Jerusalem , Israel )
- Bendor, Cole ( Hebrew University , Jerusalem , Israel )
- Libruder, Carmit ( MOH , Ramat Gan , Israel )
- Zucker, Inbar ( MOH , Ramat Gan , Israel )
- Lutski, Miri ( MOH , Ramat Gan , Israel )
Meeting Info:
Session Info:
The Threats of Hypertension to Life and Healthy Organ Function
Sunday, 11/17/2024 , 09:30AM - 10:45AM
Moderated Digital Poster Session
More abstracts on this topic:
Lee Ho-joon, Schwamm Lee, Turner Ashby, De Havenon Adam, Kamel Hooman, Brandt Cynthia, Zhao Hongyu, Krumholz Harlan, Sharma Richa
A Novel Approach to Manage Hypercholesterolemia: The Veterans Affairs Lipid Optimization Reimagined Quality Improvement (VALOR-QI) ProgramDjousse Luc, Leesch Tharen, Pena David, Gaziano Michael, Ward Rachel, Wellman Helen, Yel Nedim, Santos Abigail, Delgrande Jen, Fink Abigail, Colson Kristin, Pan Eddie
More abstracts from these authors:
Khan Sadiya, Coresh Josef
Risk scores to enable accessible precision careKhan Sadiya, Coresh Josef