Final ID: Su3074
Total Burden of Posttraumatic Stress Disorder on Incident Cardiovascular Disease Among Women Veterans
Abstract Body (Do not enter title and authors here): Introduction: Posttraumatic stress disorder (PTSD) is an independent cardiovascular disease (CVD) risk factor with high prevalence in women, particularly women veterans (WV). While the impact of PTSD on ischemic heart disease (IHD) and stroke has been well established, its impact on a comprehensive set of CVD outcomes has not been studied in WV, a growing population at high risk for CVD in the U.S. The goal of this project was to investigate the impact of PTSD on a comprehensive set of CVD conditions in WV.
Methods: National Veterans Health Affairs (VHA) electronic health records were used to identify all women who visited any VAs from 1/1/2000 to 12/31/2019. PTSD and CVD were identified based on International Classification of Disease versions 9 and 10 diagnoses ( 1 inpatient or 2 outpatient encounter documentations). Incident CVD outcomes included first onset of IHD, stroke, cardiomyopathy/heart failure (HF), pulmonary arterial hypertension/pulmonary hypertension (PH), atrial flutter/fibrillation (AF), peripheral arterial disease (PAD), venous thromboembolism (VTE), and aortic stenosis (AS). Propensity score matching and Cox survival analyses were performed to assess associations of PTSD with incident CVD outcomes.
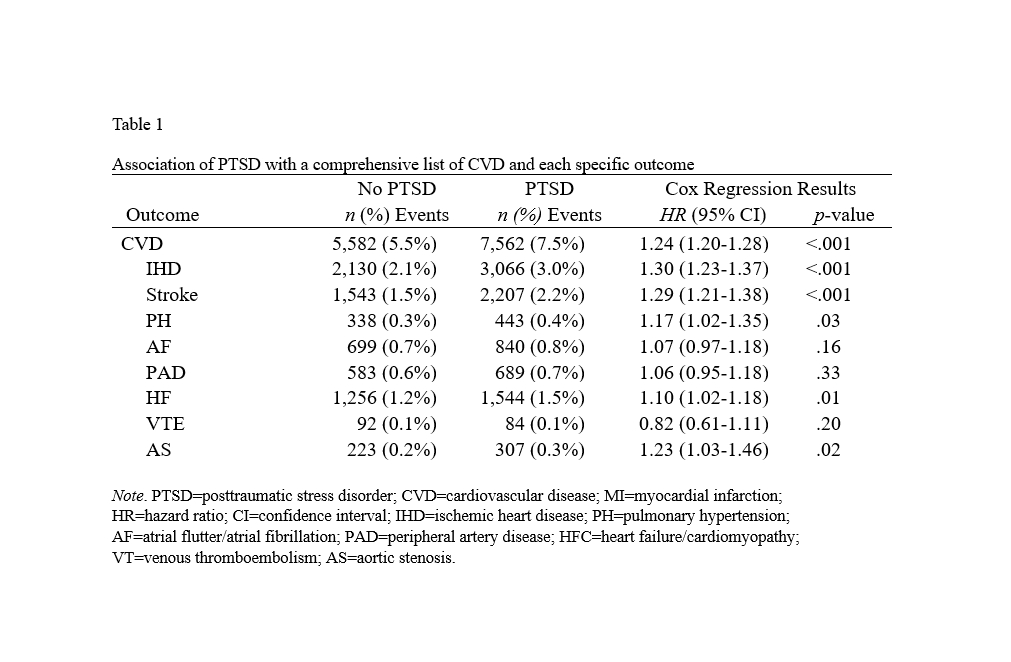
Results: We identified 622,312 WV, with 140,210 (22.53%) with PTSD. After 1:1 matching, 202,896 patients were included in the final analysis. WV had a mean age of 39.1 years, and the mean [MOU1] follow-up was 5.72 years. Table 1 reveals the association of PTSD with an incident CVD composite and the different component outcomes individually.
Conclusion: In a large sample of WV, we demonstrate significant and clinically relevant associations of PTSD with a comprehensive set of incident CVD outcomes. The potential association with some of the specific outcomes warrant further investigation. Maybe more of a call to action for PTSD screening and treatment to potentially offset CVD risk instead?
Methods: National Veterans Health Affairs (VHA) electronic health records were used to identify all women who visited any VAs from 1/1/2000 to 12/31/2019. PTSD and CVD were identified based on International Classification of Disease versions 9 and 10 diagnoses ( 1 inpatient or 2 outpatient encounter documentations). Incident CVD outcomes included first onset of IHD, stroke, cardiomyopathy/heart failure (HF), pulmonary arterial hypertension/pulmonary hypertension (PH), atrial flutter/fibrillation (AF), peripheral arterial disease (PAD), venous thromboembolism (VTE), and aortic stenosis (AS). Propensity score matching and Cox survival analyses were performed to assess associations of PTSD with incident CVD outcomes.
Results: We identified 622,312 WV, with 140,210 (22.53%) with PTSD. After 1:1 matching, 202,896 patients were included in the final analysis. WV had a mean age of 39.1 years, and the mean [MOU1] follow-up was 5.72 years. Table 1 reveals the association of PTSD with an incident CVD composite and the different component outcomes individually.
Conclusion: In a large sample of WV, we demonstrate significant and clinically relevant associations of PTSD with a comprehensive set of incident CVD outcomes. The potential association with some of the specific outcomes warrant further investigation. Maybe more of a call to action for PTSD screening and treatment to potentially offset CVD risk instead?
More abstracts on this topic:
A 50% or Greater Reduction in LDL-Cholesterol Is Associated with Improved Long-Term Outcomes and Lower Health Care Utilization After Myocardial Infarction - a SWEDEHEART study
Reitan Christian, Watanabe Alexandre, Bash Lori, Galvain Thibaut, Arnet Urs, Jernberg Tomas
A Scoping Review Exploring Cardiovascular Risk and Health Metrics and Cancer PredictionKim Ji-eun, Henriquez Santos Gretell, Kumar Sant, Livinski Alicia, Vo Jacqueline, Joo Jungnam, Shearer Joe, Hashemian Maryam, Roger Veronique