Final ID: MDP924
Trends, Outcomes and Predictors of Mortality in Patients with Myeloproliferative Neoplasms Undergoing Percutaneous Coronary Intervention: Insights from National Database
Abstract Body (Do not enter title and authors here):
Introduction
Myeloproliferative neoplasms (MPN) are stem cell disorders that include include polycythemia vera (PV), essential thrombocythemia (ET), chronic myeloid leukemia (CML), primary myelofibrosis (PMF), chronic neutrophilic leukemia, and less well defined entities such as chronic eosinophilic leukemia. MPN are associated with an increased cardiovascular risk including acute coronary syndrome. However, there is a lack of comprehensive data regarding the rate of coronary revascularization, as well as the in-hospital characteristics and outcomes for MPN patients.
Objective
We aimed to evaluate the temporal trends and outcomes of percutaneous coronary intervention (PCI) among patients with MPN.
Methods
The National Inpatient Sample database from 2016 to 2020 was queried to identify all PCI hospitalizations. Temporal trends and outcomes of patients with and without MPN following PCI were described. Propensity score matching (PSM) was implemented to compare outcomes between MPN and non-MPN groups.
Results
Our study included 2,237,210 PCI hospitalizations with 7,560 (0.27%) patients having MPN.
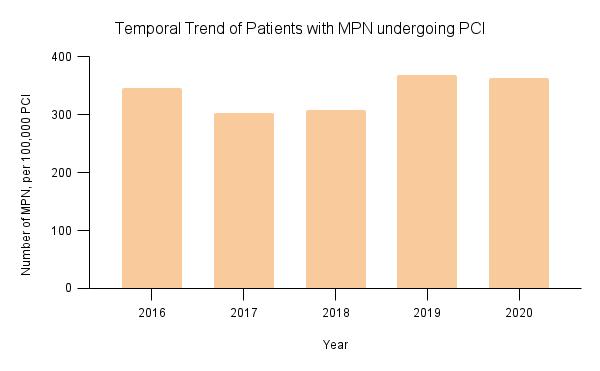
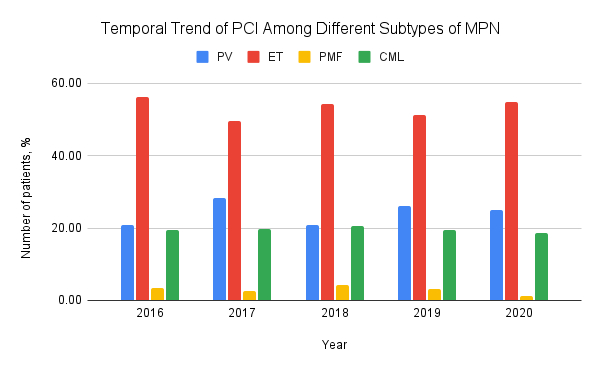
Throughout the study period, the prevalence of MPN among PCI admissions remained stable (p-value for trend = 0.12). Within the MPN subgroup, ET was the predominant condition (53.2%), followed by PV (24.2%), CML (19.6%) and PMF (3.0%), with no significant temporal variation in the distribution of these subtypes. Patients with MPN had higher prevalence of cardiovascular comorbidities than non-MPN patients. Following propensity score matching, MPNs were significantly associated with an higher risk of blood transfusions (OR: 1.66, 95% CI: 1.22-2.24, p=0.001) and AKI (OR: 1.39, 95% CI: 1.17-1.65, p<0.001). In contrast, the risk of in-hospital mortality (OR: 1.18, 95% CI: 0.83-1.69, p=0.354 and bleeding (OR: 1.43, 95% CI: 0.90-2.27, p=0.127) did not significantly differ between the two groups.
Conclusion
Our study demonstrated that while the prevalence of MPN among patients undergoing PCI remained stable, those with MPN faced higher risks of bleeding, blood transfusion and acute kidney injury. Further research is warranted to explore the underlying reasons for these increased risks and to improve outcomes in this high risk group.
Introduction
Myeloproliferative neoplasms (MPN) are stem cell disorders that include include polycythemia vera (PV), essential thrombocythemia (ET), chronic myeloid leukemia (CML), primary myelofibrosis (PMF), chronic neutrophilic leukemia, and less well defined entities such as chronic eosinophilic leukemia. MPN are associated with an increased cardiovascular risk including acute coronary syndrome. However, there is a lack of comprehensive data regarding the rate of coronary revascularization, as well as the in-hospital characteristics and outcomes for MPN patients.
Objective
We aimed to evaluate the temporal trends and outcomes of percutaneous coronary intervention (PCI) among patients with MPN.
Methods
The National Inpatient Sample database from 2016 to 2020 was queried to identify all PCI hospitalizations. Temporal trends and outcomes of patients with and without MPN following PCI were described. Propensity score matching (PSM) was implemented to compare outcomes between MPN and non-MPN groups.
Results
Our study included 2,237,210 PCI hospitalizations with 7,560 (0.27%) patients having MPN.
Throughout the study period, the prevalence of MPN among PCI admissions remained stable (p-value for trend = 0.12). Within the MPN subgroup, ET was the predominant condition (53.2%), followed by PV (24.2%), CML (19.6%) and PMF (3.0%), with no significant temporal variation in the distribution of these subtypes. Patients with MPN had higher prevalence of cardiovascular comorbidities than non-MPN patients. Following propensity score matching, MPNs were significantly associated with an higher risk of blood transfusions (OR: 1.66, 95% CI: 1.22-2.24, p=0.001) and AKI (OR: 1.39, 95% CI: 1.17-1.65, p<0.001). In contrast, the risk of in-hospital mortality (OR: 1.18, 95% CI: 0.83-1.69, p=0.354 and bleeding (OR: 1.43, 95% CI: 0.90-2.27, p=0.127) did not significantly differ between the two groups.
Conclusion
Our study demonstrated that while the prevalence of MPN among patients undergoing PCI remained stable, those with MPN faced higher risks of bleeding, blood transfusion and acute kidney injury. Further research is warranted to explore the underlying reasons for these increased risks and to improve outcomes in this high risk group.
More abstracts on this topic:
High-dimensional single-cell antibody-sequencing (AbSeq) analysis reveals age-associated myeloid cell subsets in coronary artery disease
Komaravolu Ravi, Ley Klaus, Alimadadi Ahmad, Hedrick Catherine, Chatterjee Nandini, Durant Christopher, Wu Runpei, Mcskimming Chantel, Drago Fabrizio, Taylor Angela, Mcnamara Coleen, Miller Yury
Long Duration of Type 2 Diabetes Promotes Erythrocyte-Induced Endothelial Dysfunction: Role of microRNA-210Kontidou Eftychia, Zhou Zhichao, Collado Aida, Humoud Rawan, Manickam Kesavan, Jiao Tong, Alvarsson Michael, Yang Jiangning, Mahdi Ali, Pernow John