Final ID: MDP1403
Efficacy and Safety of Sodium-Glucose Co-transporter-2 Inhibitors in Acute Heart Failure: A Meta-Analysis of Randomized Controlled Trials
Abstract Body (Do not enter title and authors here): Background:
Sodium-glucose co-transporter-2 inhibitors (SGLT2i) have demonstrated benefits in chronic heart failure. Their efficacy in acute decompensated heart failure (ADHF) is not well established, warranting further investigation. This meta-analysis evaluates the impact of SGLT2i (empagliflozin, dapagliflozin, and sotagliflozin) on patients with ADHF.
Methods:
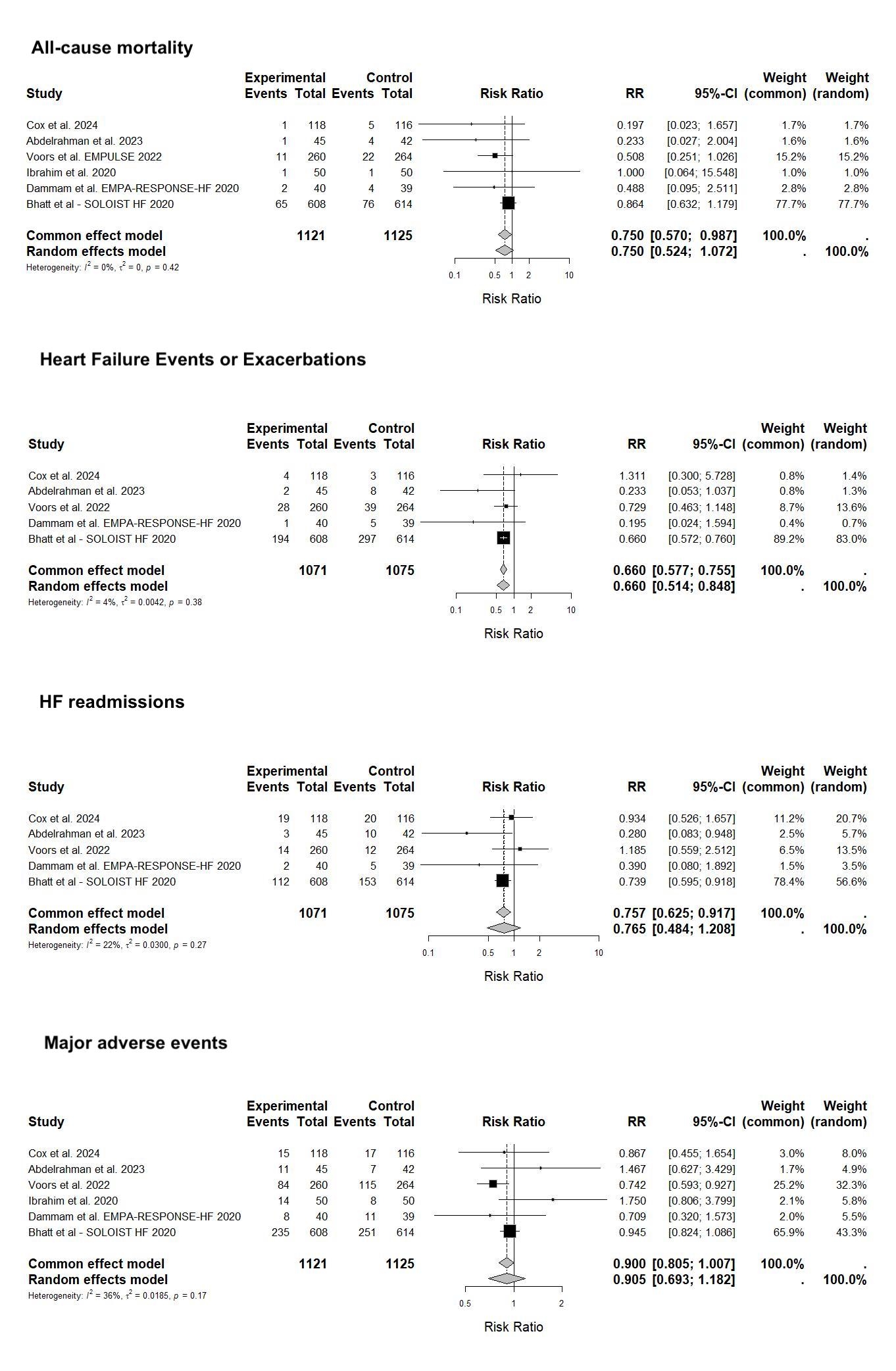
A systematic review and meta-analysis were conducted following PRISMA guidelines. Relevant studies were sourced from MEDLINE/PubMed, Scopus, and the Cochrane Central Register of Controlled Trials up to May 2024. Six studies met the inclusion criteria: Cox et al. (2024), Abdelrahman et al. (2023), Voors et al. (2022), Ibrahim et al. (2020), Dammam et al. (2020), and Bhatt et al. (2020). Three studies used dapagliflozin, two used empagliflozin, and one used sotagliflozin. Outcomes included all-cause mortality, heart failure [HF] events, HF readmissions, and major adverse events. Data analysis was performed using Microsoft Excel and R/R Studio [Version 4.4.0]. A risk ratio (RR) with 95% confidence intervals (CI) was calculated using both fixed and random effects models to assess heterogeneity.
Results:
A total of 5-6 studies were included for each outcome, with total sample sizes ranging from 2146 to 2246 participants. For all-cause mortality, the fixed effect model indicated a significant reduction by 25% (RR = 0.750, 95% CI [0.570, 0.987]), whereas the random effects model did not (RR = 0.750, 95% CI [0.524, 1.072]), with low heterogeneity. SGLT2i significantly reduced heart failure events or exacerbations in both models with a 34% reduction (RR = 0.660, 95% CI [0.577, 0.755] for fixed effect and RR = 0.660, 95% CI [0.514, 0.848] for random effects), with very low heterogeneity. Heart failure readmissions showed a significant reduction in the fixed effect model (RR = 0.757, 95% CI [0.625, 0.917]) but not in the random effects model (RR = 0.765, 95% CI [0.484, 1.208]), with moderate heterogeneity. Major adverse events showed no significant reduction in either model.
Conclusion:
SGLT2i significantly reduces heart failure events and potential readmissions in ADHF patients. The impact on all-cause mortality and major adverse events is less clear. These findings support the use of SGLT2i in heart failure management, although further research is needed to confirm benefits and identify optimal patient subgroups. Low to moderate heterogeneity supports the robustness of the results across diverse populations.
Sodium-glucose co-transporter-2 inhibitors (SGLT2i) have demonstrated benefits in chronic heart failure. Their efficacy in acute decompensated heart failure (ADHF) is not well established, warranting further investigation. This meta-analysis evaluates the impact of SGLT2i (empagliflozin, dapagliflozin, and sotagliflozin) on patients with ADHF.
Methods:
A systematic review and meta-analysis were conducted following PRISMA guidelines. Relevant studies were sourced from MEDLINE/PubMed, Scopus, and the Cochrane Central Register of Controlled Trials up to May 2024. Six studies met the inclusion criteria: Cox et al. (2024), Abdelrahman et al. (2023), Voors et al. (2022), Ibrahim et al. (2020), Dammam et al. (2020), and Bhatt et al. (2020). Three studies used dapagliflozin, two used empagliflozin, and one used sotagliflozin. Outcomes included all-cause mortality, heart failure [HF] events, HF readmissions, and major adverse events. Data analysis was performed using Microsoft Excel and R/R Studio [Version 4.4.0]. A risk ratio (RR) with 95% confidence intervals (CI) was calculated using both fixed and random effects models to assess heterogeneity.
Results:
A total of 5-6 studies were included for each outcome, with total sample sizes ranging from 2146 to 2246 participants. For all-cause mortality, the fixed effect model indicated a significant reduction by 25% (RR = 0.750, 95% CI [0.570, 0.987]), whereas the random effects model did not (RR = 0.750, 95% CI [0.524, 1.072]), with low heterogeneity. SGLT2i significantly reduced heart failure events or exacerbations in both models with a 34% reduction (RR = 0.660, 95% CI [0.577, 0.755] for fixed effect and RR = 0.660, 95% CI [0.514, 0.848] for random effects), with very low heterogeneity. Heart failure readmissions showed a significant reduction in the fixed effect model (RR = 0.757, 95% CI [0.625, 0.917]) but not in the random effects model (RR = 0.765, 95% CI [0.484, 1.208]), with moderate heterogeneity. Major adverse events showed no significant reduction in either model.
Conclusion:
SGLT2i significantly reduces heart failure events and potential readmissions in ADHF patients. The impact on all-cause mortality and major adverse events is less clear. These findings support the use of SGLT2i in heart failure management, although further research is needed to confirm benefits and identify optimal patient subgroups. Low to moderate heterogeneity supports the robustness of the results across diverse populations.
More abstracts on this topic:
Acoramidis Effect on All-Cause Mortality in Patients with p.V142I (V122I) Variant ATTR-CM: Findings From the ATTRibute-CM Study
Alexander Kevin, Bhatt Kunal, Judge Daniel, Grodin Justin, Akinboboye Olakunle, Chen Chris, Tamby Jean-francois, Castano Adam, Fox Jonathan, Fontana Marianna, Gillmore Julian, Sarswat Nitasha, Grogan Martha, Solomon Scott, Davis Margot, Cuddy Sarah, Kittleson Michelle, Shah Keyur, Griffin Jan, Ruberg Frederick, Khouri Michel
30-day and one-year outcomes of patients with severe aortic stenosis after TAVI using Myval : A Meta-analysisHasabo Elfatih A., Sultan Sherif, Soliman Osama, A. Aboali Amira, Hemmeda Lina, Salah Alaa, Alrawa Salma S., Elgadi Ammar, Abdalmotalib Malaz, Yasir H Eissa Abdullatif, Mahmmoud Fadelallah Eljack Mohammed