Final ID: Su2096
Management of Ventricular Septal Defect after Bipolar Radiofrequency Ablation for Ventricular Tachycardia
Abstract Body (Do not enter title and authors here): Background:
Ventricular septal defect (VSD) can develop as a rare complication in patients undergoing bipolar radiofrequency ablation for ventricular tachycardia (VT).
Case:
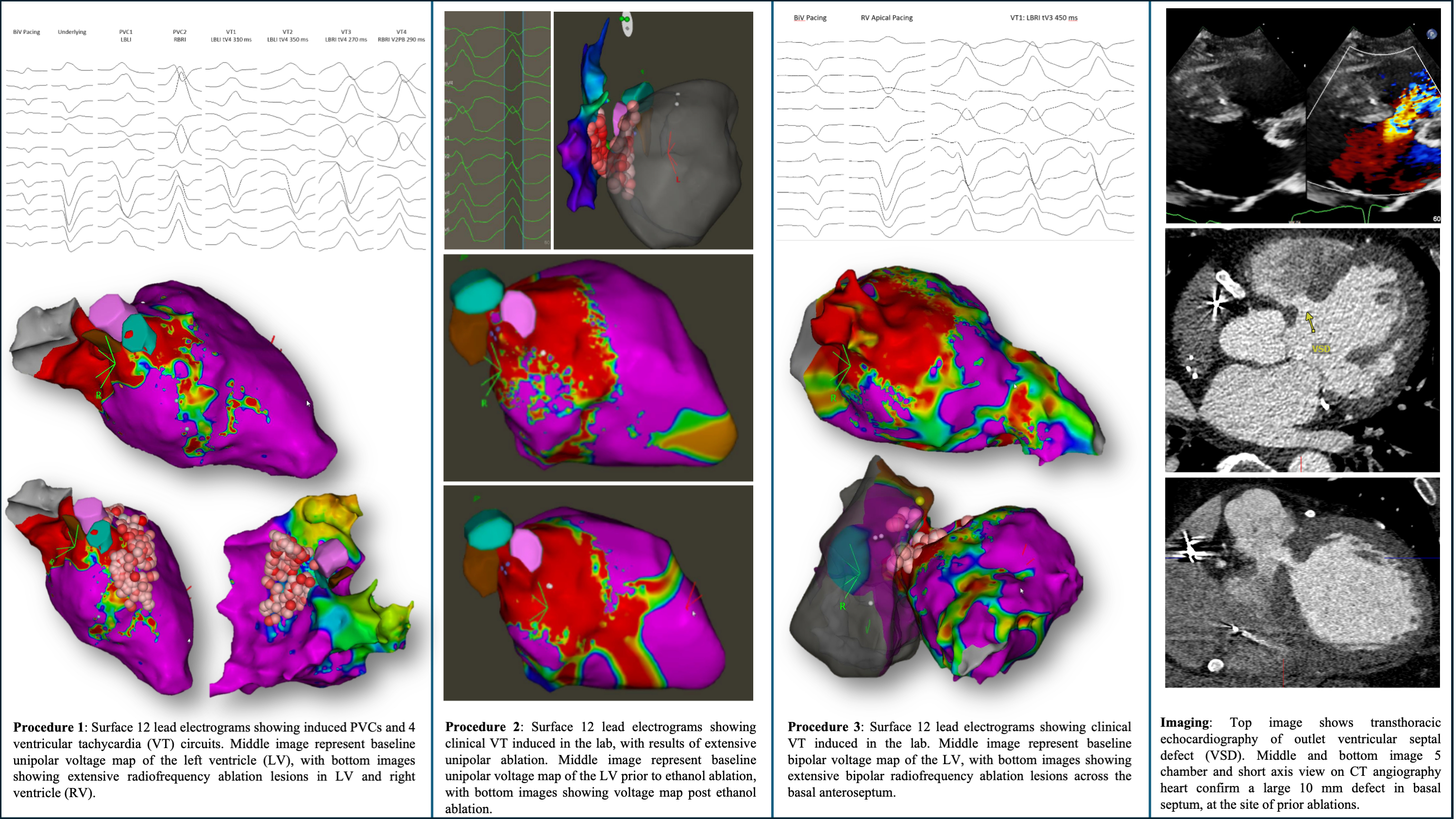
A 67-year-old male with nonischemic cardiomyopathy underwent three VT ablations over 2 years for recurrent LV summit VT. At the initial procedure, minimal bipolar voltage abnormality but significant unipolar voltage abnormality was found at the basal interventricular septum, periaortic tissue, and left ventricular (LV) summit, consistent with mid-myocardial fibrosis. Extensive endocardial unipolar radiofrequency ablation (RFA) was performed on the LV side. Despite lack of inducibility with triple extrastimuli, VT recurred that was treated with sotalol and mexiletine.
One year ago, due to recurrent symptomatic VT, he underwent a redo ablation. The clinical VT mapped earliest to the right ventricular (RV) side of basal anteroseptum. Extensive RV and LV endocardial unipolar RFA was performed, but VT remained inducible. Therefore, ethanol ablation was performed through septal perforating branch of the distal coronary sinus, after which VT could not be induced. A month later, he returned in VT storm. Repeat study mapped clinical VT earliest to the basal anteroseptal RVOT, with a focal breakout pattern on both LV and RV consistent with a deep septal substrate (earliest activation signals ~40 ms preQRS). After attempting unipolar ablation from the LV aspect, bipolar ablation was performed across the basal anterior interventricular septum. VT could no longer be induced with triple extrastimuli, on isoproterenol.
On recent routine outpatient visit 6 months later, a new murmur was noted. Multimodality imaging revealed a large (10 mm) outlet VSD in the anteroseptum with left to right shunt (Qp:Qs 1.5). LV function and cardiac index were mildly reduced (CI 2.0 ml/kg/m2). No evidence of pulmonary hypertension or RV dysfunction. After multidisciplinary heart team discussion, decision was made to attempt surgical closure.
Conclusion: Patients with refractory VT managed with multiple ablations at the same focus using different technologies should be closely monitored on an outpatient basis to evaluate for rare complications such as VSD.
Ventricular septal defect (VSD) can develop as a rare complication in patients undergoing bipolar radiofrequency ablation for ventricular tachycardia (VT).
Case:
A 67-year-old male with nonischemic cardiomyopathy underwent three VT ablations over 2 years for recurrent LV summit VT. At the initial procedure, minimal bipolar voltage abnormality but significant unipolar voltage abnormality was found at the basal interventricular septum, periaortic tissue, and left ventricular (LV) summit, consistent with mid-myocardial fibrosis. Extensive endocardial unipolar radiofrequency ablation (RFA) was performed on the LV side. Despite lack of inducibility with triple extrastimuli, VT recurred that was treated with sotalol and mexiletine.
One year ago, due to recurrent symptomatic VT, he underwent a redo ablation. The clinical VT mapped earliest to the right ventricular (RV) side of basal anteroseptum. Extensive RV and LV endocardial unipolar RFA was performed, but VT remained inducible. Therefore, ethanol ablation was performed through septal perforating branch of the distal coronary sinus, after which VT could not be induced. A month later, he returned in VT storm. Repeat study mapped clinical VT earliest to the basal anteroseptal RVOT, with a focal breakout pattern on both LV and RV consistent with a deep septal substrate (earliest activation signals ~40 ms preQRS). After attempting unipolar ablation from the LV aspect, bipolar ablation was performed across the basal anterior interventricular septum. VT could no longer be induced with triple extrastimuli, on isoproterenol.
On recent routine outpatient visit 6 months later, a new murmur was noted. Multimodality imaging revealed a large (10 mm) outlet VSD in the anteroseptum with left to right shunt (Qp:Qs 1.5). LV function and cardiac index were mildly reduced (CI 2.0 ml/kg/m2). No evidence of pulmonary hypertension or RV dysfunction. After multidisciplinary heart team discussion, decision was made to attempt surgical closure.
Conclusion: Patients with refractory VT managed with multiple ablations at the same focus using different technologies should be closely monitored on an outpatient basis to evaluate for rare complications such as VSD.
More abstracts on this topic:
Ablation versus Anti-arrhythmic Drug Therapy for Ventricular Tachycardia in Patients with Ischemic Heart Disease: A Systematic Review and Meta-analysis of Randomized Controlled Trials
Khan Ubaid, Chaudhry Kashif, Amin Ahmed Mazen, A. Ibrahim Ahmed, Imran Muhammad, Rakab Mohamed, Iltaf Arej, M. Albarakat Majd, Ranabhat Chet, Brilliant Justin
Association Between Left Atrial Conduction Velocity and Atrial Fibrillation Recurrence After Pulmonary Vein Isolation Alone Using Radiofrequency Catheter Ablation: A Meta-Analysis and Diagnostic Accuracy StudyOdat Ramez, Gharaibeh Ahmad, Aldamen Ali, Jain Hritvik, Altarawneh Tala, Rhabneh Laith, Soni Kriti, Agrawal Siddharth, Patel Bhavin, Aqtash Obadah