Final ID: MDP944
Predictors of Developing Ischemia-Reperfusion Injury Immediately after Heart Transplantation
Abstract Body (Do not enter title and authors here): Introduction: Post-heart Transplant (HTx) ischemia-reperfusion injury (IRI) is not uncommon and has been associated with an increased risk of rejection and cardiac allograft vasculopathy. IRI may occur due to long ischemia time, high dose inotropes, and technical surgical reasons. Identifying other recipient and donor characteristics that might set patients at higher risk for developing IRI might help inform decision-making and improve patient outcomes. Therefore, we aim to investigate predictors of developing IRI immediately after HTx.
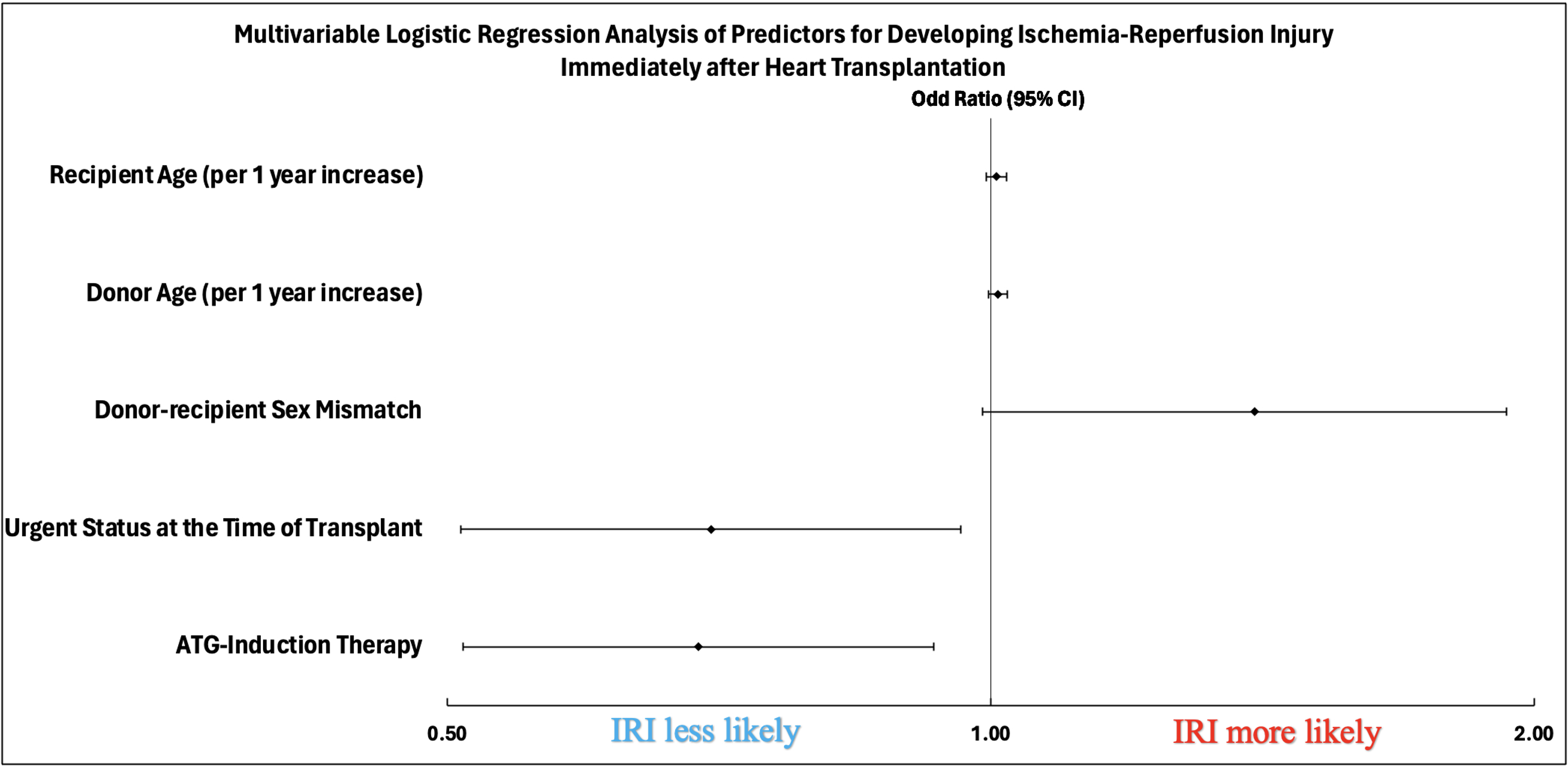
Methods: Between 2010 and 2020, we assessed 893 patients undergoing HTx at our center. Recipient and donor characteristics were collected and compared between patients who were noted to have immediate post-HTx (within 30 days) IRI on their endomyocardial biopsy (n=241) vs. those who did not (n=652). Multivariable logistic regression was used to determine predictors of IRI development and included all univariate significant variables with (P<0.1). Outcomes were represented as odds ratios with corresponding 95% confidence intervals.
Results: Among 893 patients undergoing HTx, 241 (27%) had IRI within 30 days post-HTx (time to IRI was 14.4 ± 7.3 days). Compared to patients without IRI, those who developed IRI trended towards being older (57 ± 12 vs. 55 ±13 years, P=0.07), were less likely to receive induction therapy with anti-thymocyte globulin (ATG) (43.6 vs. 52.9%, P=0.01), and less likely to be listed with an urgent status at the time of HTx (62.7% vs. 71.9%, P=0.008). Patients listed with an urgent status were on optimal hemodynamic support. No other significant differences were recorded in other pre-transplant or peri-operative recipient characteristics among patients who developed IRI vs. those who did not. In regard to donor characteristics, those who developed IRI received hearts from older donors (37 ± 13.5 vs. 34.9 ± 12.2, P=0.03) and showed a trend toward a higher likelihood of donor-recipient sex mismatch (29.9% vs. 23.6%, P=0.059), regardless of recipient sex. On multivariable logistic regression, only ATG-induction [OR:0.69, 95%CI [0.51-0.93], P=0.015) therapy and urgent status at transplantation [OR:07, 95%CI [0.51-0.96], P=0.028) were significant predictors of IRI development
Conclusion: Optimal prioritization of HTx candidates on the waitlist and use of ATG induction therapy seem to protect against immediate IRI post-HTx.
Methods: Between 2010 and 2020, we assessed 893 patients undergoing HTx at our center. Recipient and donor characteristics were collected and compared between patients who were noted to have immediate post-HTx (within 30 days) IRI on their endomyocardial biopsy (n=241) vs. those who did not (n=652). Multivariable logistic regression was used to determine predictors of IRI development and included all univariate significant variables with (P<0.1). Outcomes were represented as odds ratios with corresponding 95% confidence intervals.
Results: Among 893 patients undergoing HTx, 241 (27%) had IRI within 30 days post-HTx (time to IRI was 14.4 ± 7.3 days). Compared to patients without IRI, those who developed IRI trended towards being older (57 ± 12 vs. 55 ±13 years, P=0.07), were less likely to receive induction therapy with anti-thymocyte globulin (ATG) (43.6 vs. 52.9%, P=0.01), and less likely to be listed with an urgent status at the time of HTx (62.7% vs. 71.9%, P=0.008). Patients listed with an urgent status were on optimal hemodynamic support. No other significant differences were recorded in other pre-transplant or peri-operative recipient characteristics among patients who developed IRI vs. those who did not. In regard to donor characteristics, those who developed IRI received hearts from older donors (37 ± 13.5 vs. 34.9 ± 12.2, P=0.03) and showed a trend toward a higher likelihood of donor-recipient sex mismatch (29.9% vs. 23.6%, P=0.059), regardless of recipient sex. On multivariable logistic regression, only ATG-induction [OR:0.69, 95%CI [0.51-0.93], P=0.015) therapy and urgent status at transplantation [OR:07, 95%CI [0.51-0.96], P=0.028) were significant predictors of IRI development
Conclusion: Optimal prioritization of HTx candidates on the waitlist and use of ATG induction therapy seem to protect against immediate IRI post-HTx.
More abstracts on this topic:
A Heart Transplant Patient’s Mysterious Illness: A Diagnostic Odyssey
Alkalbani Mutaz, Nayer Hassan, Cochrane Adam, Saeed Ibrahim, Psotka Mitchell, Rollins Allman, Kennedy Jamie, Blumer Vanessa
Assessment of Adverse Left Ventricular Remodeling Following Ischemia Reperfusion Injury with SPECT Imaging Agent Targeting Fibroblast Activation ProteinThorn Stephanie, Duncan James S, Spinale Francis, Luna Gutierrez Myrna, Ferro-flores Guillermina, Sinusas Albert, Porcaro Olivia, Burns Rachel, Zohora Fatema Tuj, Guerrera Nicole, Jang Sun-joo, Vermillion Billy, Lima Moroni, Liu Chi