Final ID: MDP1632
Trends in Stimulant-Involved Cardiovascular Disease Mortality, 1999 – 2023
Abstract Body (Do not enter title and authors here): Introduction: Cocaine and methamphetamine, stimulants with potent central nervous system effects, are known to be cardiotoxic. They increase the risk of hypertension, coronary artery disease, coronary vasospasm, arrhythmias, cardiomyopathy, cardiac arrest, and stroke. Despite these well-documented risks, the National Survey on Drug Use and Health reports that illicit stimulant use is increasing.
Research Question: How have mortality rates changed over time when cardiovascular disease (CVD) is the underlying cause of death and illicit stimulant use is a contributing factor?
Aims: To describe trends in cardiovascular mortality rates from 1999-2023 and to stratify the analysis by race, ethnicity, sex, age, CVD subcategories, and stimulant type.
Methods: We leveraged CDC WONDER data to model age-adjusted CVD mortality rates from 1999 to 2023 using joinpoint regression. For each stimulant type, demographic group, and CVD subcategory, we report annual percent changes (APCs) for each time segment and average annual percent changes (AAPCs) to estimate overall trend direction and magnitude.
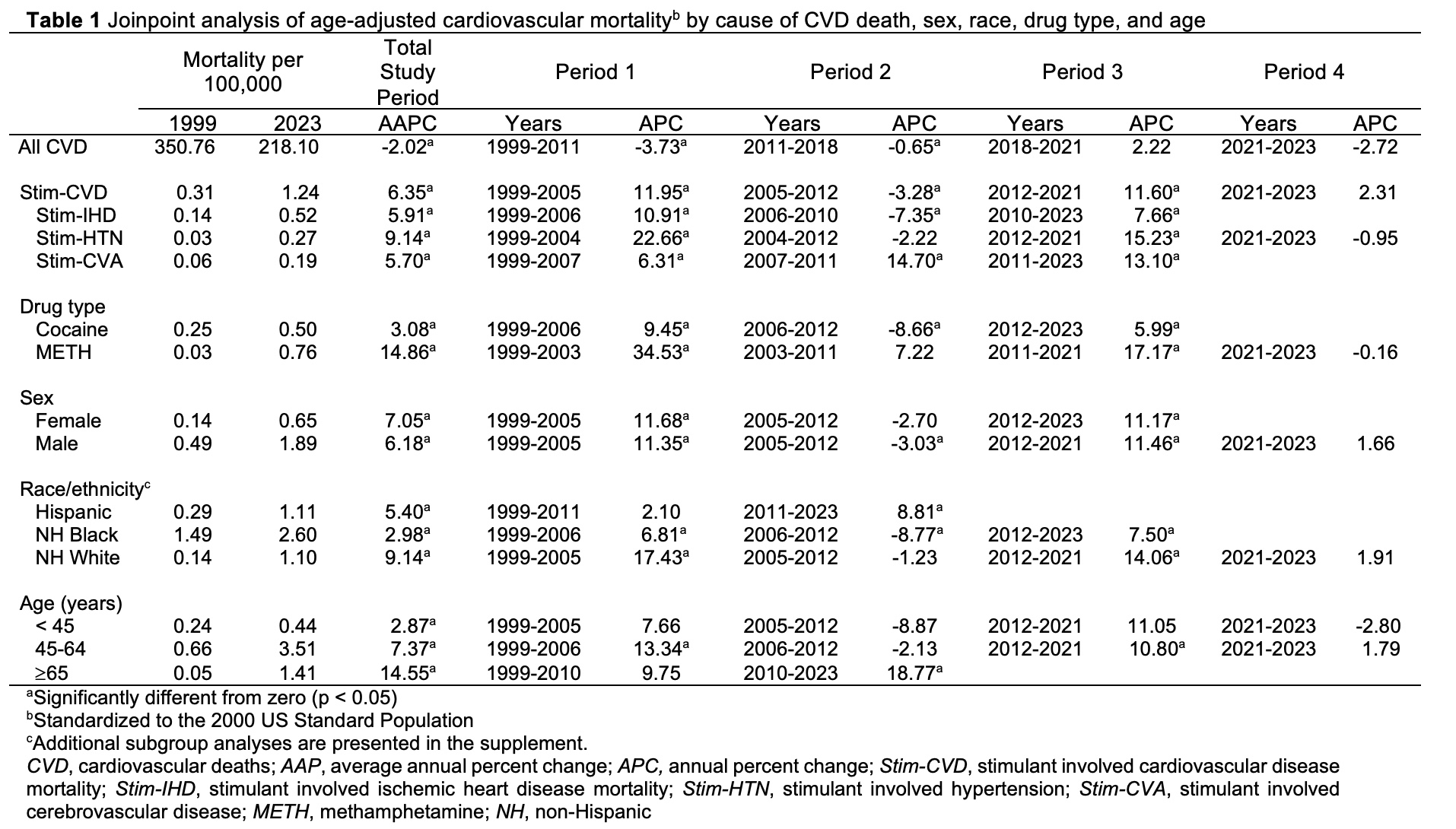
Results: From 1999 to 2023, stimulant-involved CVD mortality rates increased significantly, with an AAPC of 6.4%, contrasting sharply with the 2.0% decline in overall CVD mortality rates (Table). Each subcategory of CVD mortality (ischemic heart disease, hypertension; cerebrovascular disease) showed AAPC increases when stimulants were involved, with hypertensive diseases experiencing the largest AAPC rise at 9.1%.
Stratifying by drug type, methamphetamine-involved CVD death rates increased by 14.9% AAPC, compared to a 3.1% increase for cocaine-involved deaths. Demographic stratification revealed additional differences. Non-Hispanic White individuals had the highest AAPC (9.2%), followed by Asian/Pacific Islander (5.6%), Hispanic (5.4%), Non-Hispanic Black (3.0%), and American Indian/Alaskan Native individuals (1.9%). A higher AAPC also was observed among those aged ≥65 years (14.6%).
Conclusions: Cardiovascular deaths where stimulants were a contributing cause have increased rapidly over the past 25 years despite the overall decline in the CVD mortality rate during the same period. The largest increases were seen in hypertensive diseases, methamphetamine-involved deaths, non-Hispanic White individuals, and older individuals. This study extends our understanding but is limited by potential inaccuracies in the recorded causes of death.
Research Question: How have mortality rates changed over time when cardiovascular disease (CVD) is the underlying cause of death and illicit stimulant use is a contributing factor?
Aims: To describe trends in cardiovascular mortality rates from 1999-2023 and to stratify the analysis by race, ethnicity, sex, age, CVD subcategories, and stimulant type.
Methods: We leveraged CDC WONDER data to model age-adjusted CVD mortality rates from 1999 to 2023 using joinpoint regression. For each stimulant type, demographic group, and CVD subcategory, we report annual percent changes (APCs) for each time segment and average annual percent changes (AAPCs) to estimate overall trend direction and magnitude.
Results: From 1999 to 2023, stimulant-involved CVD mortality rates increased significantly, with an AAPC of 6.4%, contrasting sharply with the 2.0% decline in overall CVD mortality rates (Table). Each subcategory of CVD mortality (ischemic heart disease, hypertension; cerebrovascular disease) showed AAPC increases when stimulants were involved, with hypertensive diseases experiencing the largest AAPC rise at 9.1%.
Stratifying by drug type, methamphetamine-involved CVD death rates increased by 14.9% AAPC, compared to a 3.1% increase for cocaine-involved deaths. Demographic stratification revealed additional differences. Non-Hispanic White individuals had the highest AAPC (9.2%), followed by Asian/Pacific Islander (5.6%), Hispanic (5.4%), Non-Hispanic Black (3.0%), and American Indian/Alaskan Native individuals (1.9%). A higher AAPC also was observed among those aged ≥65 years (14.6%).
Conclusions: Cardiovascular deaths where stimulants were a contributing cause have increased rapidly over the past 25 years despite the overall decline in the CVD mortality rate during the same period. The largest increases were seen in hypertensive diseases, methamphetamine-involved deaths, non-Hispanic White individuals, and older individuals. This study extends our understanding but is limited by potential inaccuracies in the recorded causes of death.
More abstracts on this topic:
A cerebrovascular longitudinal atlas: different rates of morphological change in aneurysm patients associated with hypertension and diabetes
Chien Aichi, Salamon Noriko, Vinuela Fernando, Szeder Viktor, Colby Geoffrey, Jahan Reza, Boyle Noel, Villablanca Juan, Duckwiler Gary
Advancing towards the development of an AI application for angina diagnosis through medical interviewsFujita Kosuke, Shoda Yudai, Kanno Honoka, Handa Hisashi, Nakazawa Gaku