Final ID: MDP1114
Glucagon-like peptide-1 Receptor Agonists reduce the Incidence of Echocardiographic Pulmonary Hypertension
Abstract Body (Do not enter title and authors here):
Introduction:
No interventions decrease the risk of developing pulmonary hypertension (PH). We hypothesize Glucagon-like peptide-1 receptor agonists (GLP-1) reduce risk of PH through salutary changes in metabolism, weight, and the pulmonary vasculature. We examined GLP-1 exposure and development of PH among pts with diabetes (DM) in a national healthcare system.
Methods:
Pulmonary artery systolic pressure (PASP) estimates were extracted from TTEs in the Veterans Affairs system. PH (primary outcome) was defined as PASP >35 mmHg. Individuals free of PH on or after 1/2007 (baseline) were followed through the development of PH, death, or censored on 12/2020. The primary exposure was GLP-1 prescription modeled as: 1) Baseline exposure 2) Time-updated exposure and 3) Cumulative days of exposure (among exposed). We used multivariable cox models adjusted for demographics, comorbidities, and clinical characteristics in Table 1.
Results:
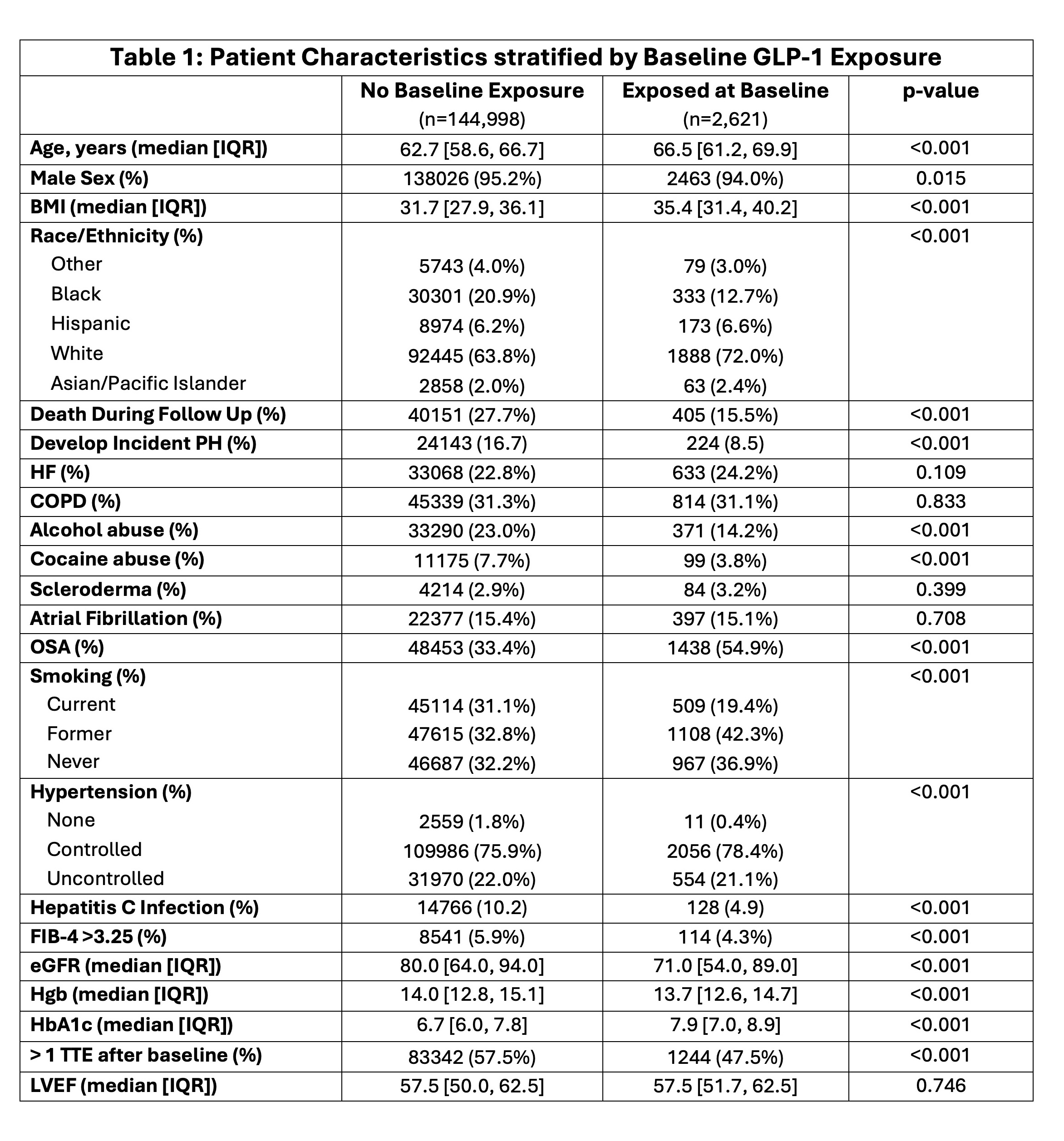
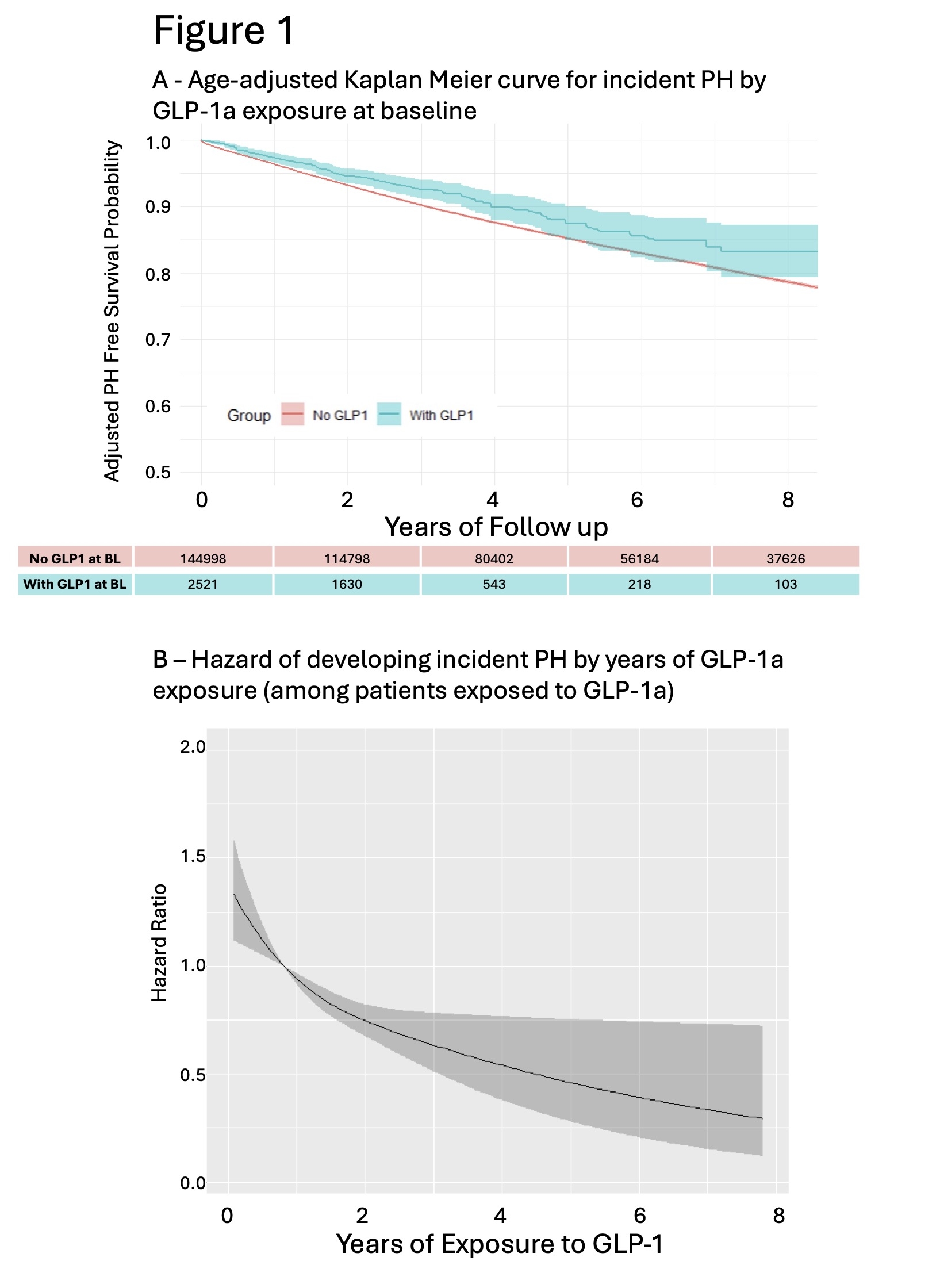
We identified 147,619 patients with DM (63 years [IQR 59-67], 95% Male, 21% Black) with a baseline TTE free of PH. Median follow up was 4.5 years (2.3-7.3 IQR). Of these, 2,621 pts were exposed to GLP-1 at baseline and 5,699 pts after baseline. Median time on drug (among exposed) was 296 days (120-570 IQR). Characteristics of exposed vs unexposed at baseline are displayed in Table 1 with Age-adjusted Kaplan Meier curve in Figure 1A. GLP-1 exposure associated with decreased risk of incident PH when modeled as baseline exposure (HR 0.76; 95% CI 0.67-0.87), time-varying exposure (HR 0.82; 95% CI 0.76-0.89), and time-varying exposure restricted to pts without baseline exposure (HR 0.85; 95% CI 0.78-0.94). Risk of PH decreased as days on GLP-1 increased (Figure 1B). At 90 days on drug, we observed decreased risk of PH (HR 0.94; 95%CI 0.92-0.96).
Conclusions:
GLP-1 exposure at baseline or de novo during follow up is associated with decreased incidence of PH in pts with DM. The benefit from GLP-1 starts near 90 days and increases with time on drug.
Introduction:
No interventions decrease the risk of developing pulmonary hypertension (PH). We hypothesize Glucagon-like peptide-1 receptor agonists (GLP-1) reduce risk of PH through salutary changes in metabolism, weight, and the pulmonary vasculature. We examined GLP-1 exposure and development of PH among pts with diabetes (DM) in a national healthcare system.
Methods:
Pulmonary artery systolic pressure (PASP) estimates were extracted from TTEs in the Veterans Affairs system. PH (primary outcome) was defined as PASP >35 mmHg. Individuals free of PH on or after 1/2007 (baseline) were followed through the development of PH, death, or censored on 12/2020. The primary exposure was GLP-1 prescription modeled as: 1) Baseline exposure 2) Time-updated exposure and 3) Cumulative days of exposure (among exposed). We used multivariable cox models adjusted for demographics, comorbidities, and clinical characteristics in Table 1.
Results:
We identified 147,619 patients with DM (63 years [IQR 59-67], 95% Male, 21% Black) with a baseline TTE free of PH. Median follow up was 4.5 years (2.3-7.3 IQR). Of these, 2,621 pts were exposed to GLP-1 at baseline and 5,699 pts after baseline. Median time on drug (among exposed) was 296 days (120-570 IQR). Characteristics of exposed vs unexposed at baseline are displayed in Table 1 with Age-adjusted Kaplan Meier curve in Figure 1A. GLP-1 exposure associated with decreased risk of incident PH when modeled as baseline exposure (HR 0.76; 95% CI 0.67-0.87), time-varying exposure (HR 0.82; 95% CI 0.76-0.89), and time-varying exposure restricted to pts without baseline exposure (HR 0.85; 95% CI 0.78-0.94). Risk of PH decreased as days on GLP-1 increased (Figure 1B). At 90 days on drug, we observed decreased risk of PH (HR 0.94; 95%CI 0.92-0.96).
Conclusions:
GLP-1 exposure at baseline or de novo during follow up is associated with decreased incidence of PH in pts with DM. The benefit from GLP-1 starts near 90 days and increases with time on drug.
More abstracts on this topic:
AAV-mediated Gene Delivery of PERM1 Prevents the Development of Heart Failure with Reduced Ejection Fraction in a Mouse Model of Pressure Overload
Sreedevi Karthi, Doku Abigail Oforiwaa, Thomas Rebekah, Salama Sarah, Zaitsev Alexey, Warren Junco
A single-cell lung atlas of human pulmonary arterial hypertensionDai Zhiyu, Yi Dan, Zhao Hanqiu, Hong Jason, Fallon Michael