Final ID: 4139555
Transitions Between Heart Failure States in Adult Patients with Congenital Heart Disease
Abstract Body (Do not enter title and authors here): Background: The growing number of adult congenital heart disease (CHD) patients facing heart failure (HF) related complications after the age of 40 has become a major concern. There is a lack of data to capture the dynamic nature of HF progression across the adulthood, with the consideration of various contributing factors. This application of multistate models paves a promising way to accurately track health state changes, thus to provide data to inform surveillance and interventions to prevent disease progression, potentially improving personalized treatment plans for a significant patient population.
Aims: This study aimed to (1) determine the expected time a patient remains in each HF state, based on predisposing factors; (2) evaluate the probabilities that, across different ages, a patient will either remain at the same state, transition to the next HF state, or die; (3) identify the risk factors of transitioning between health states related to HF among CHD patients.
Methods: The dataset was derived from the Quebec CHD database which encompasses 137,493 patients, spanning 35 years of follow-up from 1983 to 2017. We constructed a multistate model to include 6 states: no HF history (0HF), having one (1HF), two (2HF), three (3HF) or more than four HF events (4+HF), and death. Each HF state transition was modeled by Cox proportional hazards regression using the same predictors, including sex, presence of severe congenital heart defects, and comorbidity history.
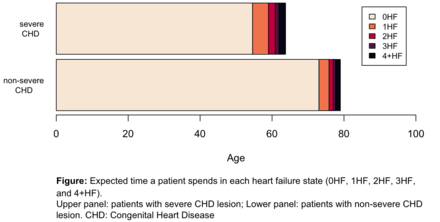
Results: The study included 83,669 adult patients with CHD. Among them, 32,934 HF events and 16,348 deaths were observed during a total of 1,732,942 person-years of follow-up. With each HF occurrence, patients showed faster progression to subsequent HF events. Patients with severe CHD lesion had nearly two decades fewer HF-free years compared to those with non-severe lesions (Figure). Early age of initial HF increased the risk of additional HF events and mortality. Comorbidities such as diabetes and chronic kidney disease markedly reduced the duration that a CHD patient remains HF-free.
Conclusion: The study findings highlight the need for early intervention and personalized treatment strategies in managing HF progression in CHD patients.
Aims: This study aimed to (1) determine the expected time a patient remains in each HF state, based on predisposing factors; (2) evaluate the probabilities that, across different ages, a patient will either remain at the same state, transition to the next HF state, or die; (3) identify the risk factors of transitioning between health states related to HF among CHD patients.
Methods: The dataset was derived from the Quebec CHD database which encompasses 137,493 patients, spanning 35 years of follow-up from 1983 to 2017. We constructed a multistate model to include 6 states: no HF history (0HF), having one (1HF), two (2HF), three (3HF) or more than four HF events (4+HF), and death. Each HF state transition was modeled by Cox proportional hazards regression using the same predictors, including sex, presence of severe congenital heart defects, and comorbidity history.
Results: The study included 83,669 adult patients with CHD. Among them, 32,934 HF events and 16,348 deaths were observed during a total of 1,732,942 person-years of follow-up. With each HF occurrence, patients showed faster progression to subsequent HF events. Patients with severe CHD lesion had nearly two decades fewer HF-free years compared to those with non-severe lesions (Figure). Early age of initial HF increased the risk of additional HF events and mortality. Comorbidities such as diabetes and chronic kidney disease markedly reduced the duration that a CHD patient remains HF-free.
Conclusion: The study findings highlight the need for early intervention and personalized treatment strategies in managing HF progression in CHD patients.
More abstracts on this topic:
β1 Adrenergic Receptor Autoantibodies Promote Heart Failure Though Activation of Prostaglandin E2 Receptor EP1/Phosphodiesterase 4B Pathway
Cao Ning, Qiu Hui, Li Hongwei
22q11 Deletion Syndrome: A Potenitial Risk Factor For Left Pulmonary Artery Hypoplasia and Need For Intervention in Patients With Congeital Heart DiseaseOliver Shannon, Ward Cameron