Final ID: MDP585
Prognostic Characteristics of Patients with Electrocardiograms Masquerading as ST Elevation Myocardial Infarction
Abstract Body (Do not enter title and authors here): Background:
Prehospital identification of STEMI reduces time to reperfusion by timely primary PCI or fibrinolytic therapy. We previously reported that 40-50% of prehospital ECG transmissions meeting Glasgow algorithm (GA) criteria for STEMI did not meet STEMI criteria on adjudication using the 4th Universal Definition of MI (4UDMI). These cases, herewith called ‘masquerading STEMI’, had high rates of late clinical complications. Here, we determined clinical factors predictive of late clinical outcomes among patients with masquerading STEMI.
Methods:
From June 2010 to October 2021, 2,992 patients with prehospital ECG transmissions to Liverpool Hospital, Sydney, Australia, who met GA criteria for STEMI were identified. These were adjudicated according to the 4UDMI as confirmed STEMI or masquerading STEMI. Using multivariate logistic regression, we identified baseline patient characteristics that were associated with the outcome of cardiovascular death, MI and stroke at 2 years, among the masquerading STEMI cohort.
Results:
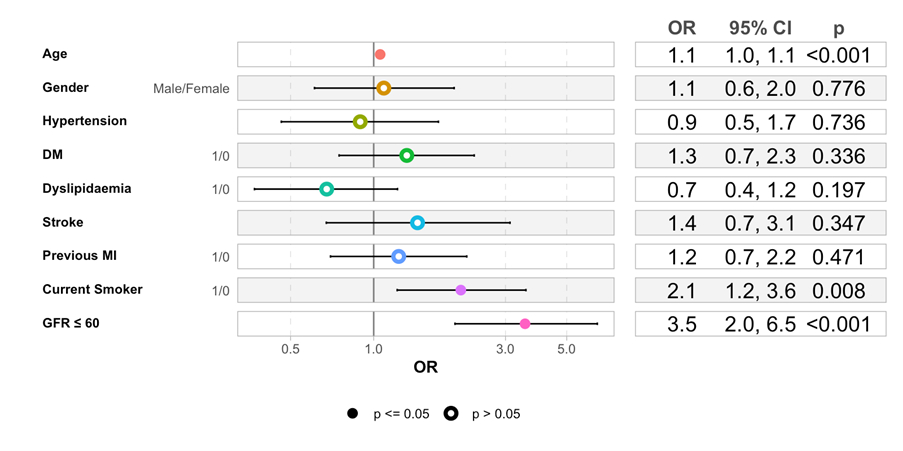
1553 (51%) patients were true-positive STEMI, while 1439 (49%) were masquerading STEMI. In the masquerading STEMI cohort, age, current smoking, and CKD (eGFR<60) were significant predictors of the 2-year cardiovascular death, MI stroke with OR of 1.05, 2.07, and 3.58, respectively (p<0.05 for all). Diabetes predicted MI re-presentation within 2 years (OR 3.76, p<0.05), and CKD predicted heart failure hospitalisation (OR 2.55, p<0.05).
Conclusions:
Among patients with masquerading STEMI, current smoking and CKD were associated with the 2-year cardiovascular death, MI stroke. Diabetes predicted a higher risk of re-presenting with MI within 2 years, and CKD predicted a higher risk of hospitalisation with heart failure. Therefore, in this cohort of patients with masquerading STEMI, despite not having a true STEMI, smoking cessation and opportunistic management of diabetes and CKD may modify prognosis.
Prehospital identification of STEMI reduces time to reperfusion by timely primary PCI or fibrinolytic therapy. We previously reported that 40-50% of prehospital ECG transmissions meeting Glasgow algorithm (GA) criteria for STEMI did not meet STEMI criteria on adjudication using the 4th Universal Definition of MI (4UDMI). These cases, herewith called ‘masquerading STEMI’, had high rates of late clinical complications. Here, we determined clinical factors predictive of late clinical outcomes among patients with masquerading STEMI.
Methods:
From June 2010 to October 2021, 2,992 patients with prehospital ECG transmissions to Liverpool Hospital, Sydney, Australia, who met GA criteria for STEMI were identified. These were adjudicated according to the 4UDMI as confirmed STEMI or masquerading STEMI. Using multivariate logistic regression, we identified baseline patient characteristics that were associated with the outcome of cardiovascular death, MI and stroke at 2 years, among the masquerading STEMI cohort.
Results:
1553 (51%) patients were true-positive STEMI, while 1439 (49%) were masquerading STEMI. In the masquerading STEMI cohort, age, current smoking, and CKD (eGFR<60) were significant predictors of the 2-year cardiovascular death, MI stroke with OR of 1.05, 2.07, and 3.58, respectively (p<0.05 for all). Diabetes predicted MI re-presentation within 2 years (OR 3.76, p<0.05), and CKD predicted heart failure hospitalisation (OR 2.55, p<0.05).
Conclusions:
Among patients with masquerading STEMI, current smoking and CKD were associated with the 2-year cardiovascular death, MI stroke. Diabetes predicted a higher risk of re-presenting with MI within 2 years, and CKD predicted a higher risk of hospitalisation with heart failure. Therefore, in this cohort of patients with masquerading STEMI, despite not having a true STEMI, smoking cessation and opportunistic management of diabetes and CKD may modify prognosis.
More abstracts on this topic:
A Case of Myocardial Infarction with Non-obstructive Coronary Arteries (MINOCA) Complicated by a Ventricular Septal Defect (VSD)
Thai Theresa, Lipinski Jerry, Sola Michael, El Rafei Abdelghani, Desai Aken, Sailer Christine
Angiographic and Clinical Outcomes with Drug-Coated Balloon Versus Drug-Eluting Stents for In-Stent Restenosis: A Meta-AnalysisJain Hritvik, Passey Siddhant, Odat Ramez, Pervez Neha, Goyal Aman, Jain Jyoti, Patel Nandan, Yadav Ashish, Shah Janhvi, Jha Jagriti