Final ID: MDP1171
Atrial Fibrillation Wave Vectors Determined by Artificial-Intelligence Indicate Clinical Phenotypes
Abstract Body (Do not enter title and authors here): Background:
Atrial fibrillation (AF) is a major cause of morbidity and mortality, which may be reduced by ablation. However, it is difficult to predict patients who will respond, which is currently done using bedside variables since even experts find it difficult to interpret electrical signals (electrograms) or maps in AF, or link them with phenotype, acute or long-term ablation response.
Hypothesis:
We hypothesized that determining if AF waves consistently propagate away from the pulmonary veins (PV), identified using artificial-intelligence (AI) tools applied to spatial grids in multipolar catheters, may reflect phenotypes of response to ablation or other clinical features.
Methods:
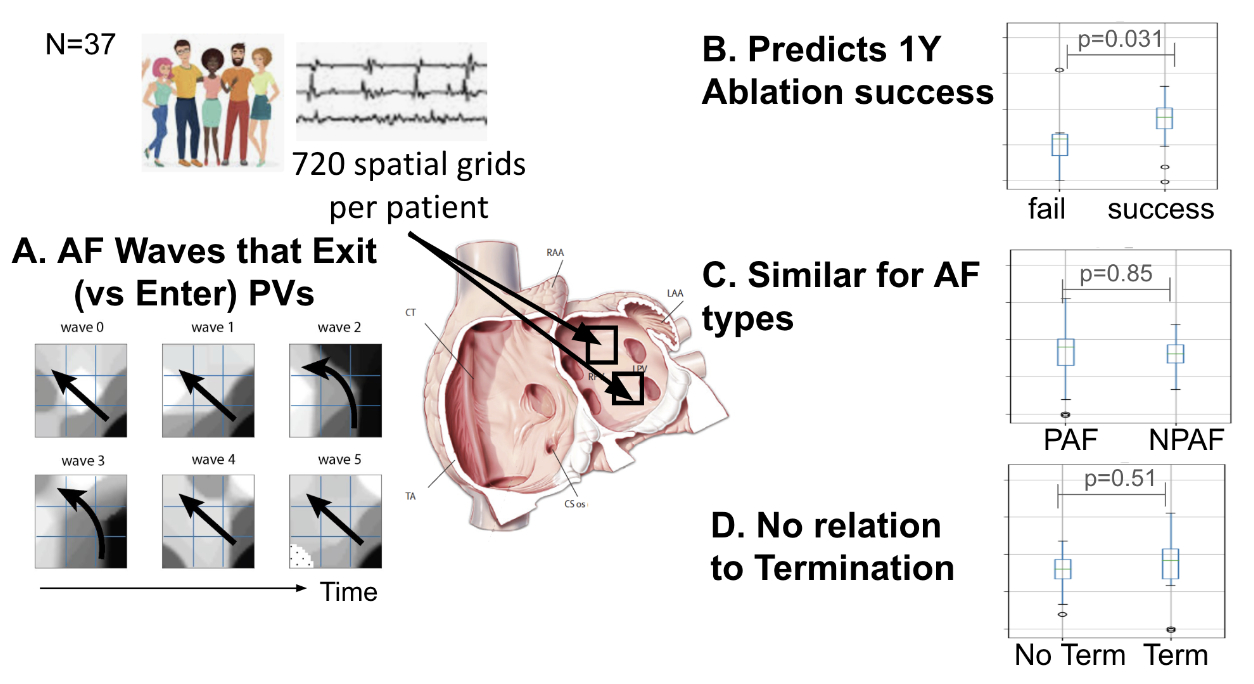
We studied 26,640 electrograms in N=37 patients at AF ablation ( 66.3 ± 8.6 years, 13.5% women, 59.5% non-paroxysmal AF). We trained AI-algorithms to identify activation patterns and calculate propagation vectors in AF. Each patient had AF recordings from 64-pole basket catheters, from which we calculated AI-based vectors in 48 spatial grids of 3X3 electrodes (covering ~1-3 cm2) over 1 minute (720 per patient). Fig. A illustrates AF waves predominantly exiting the PVs in a 60 year old man. We studied wave maps exiting the PVs in relation to AF type, termination of AF during ablation and 1 year outcome.
Results:
Ablation success for the cohort was 71.4% at 1 year. Wave direction in AF shifted over time, as expected, but predominant vectors correlated with clinical outcomes. Fig. B showed that AF waves were significantly more likely to exit the PVs for patients with success than failed ablation (<0.05). Fig. C showed that PV wave direction did not differ for AF type, nor for patients with or without acute AF termination by ablation (p=NS).
Conclusions:
In this study of patients with various types of AF, a novel AI-based approach showed that AF vectors indicating waves exiting the PVs predicted , clinical phenotypes, particularly patients with successful ablation targeting the PVs.
Atrial fibrillation (AF) is a major cause of morbidity and mortality, which may be reduced by ablation. However, it is difficult to predict patients who will respond, which is currently done using bedside variables since even experts find it difficult to interpret electrical signals (electrograms) or maps in AF, or link them with phenotype, acute or long-term ablation response.
Hypothesis:
We hypothesized that determining if AF waves consistently propagate away from the pulmonary veins (PV), identified using artificial-intelligence (AI) tools applied to spatial grids in multipolar catheters, may reflect phenotypes of response to ablation or other clinical features.
Methods:
We studied 26,640 electrograms in N=37 patients at AF ablation ( 66.3 ± 8.6 years, 13.5% women, 59.5% non-paroxysmal AF). We trained AI-algorithms to identify activation patterns and calculate propagation vectors in AF. Each patient had AF recordings from 64-pole basket catheters, from which we calculated AI-based vectors in 48 spatial grids of 3X3 electrodes (covering ~1-3 cm2) over 1 minute (720 per patient). Fig. A illustrates AF waves predominantly exiting the PVs in a 60 year old man. We studied wave maps exiting the PVs in relation to AF type, termination of AF during ablation and 1 year outcome.
Results:
Ablation success for the cohort was 71.4% at 1 year. Wave direction in AF shifted over time, as expected, but predominant vectors correlated with clinical outcomes. Fig. B showed that AF waves were significantly more likely to exit the PVs for patients with success than failed ablation (<0.05). Fig. C showed that PV wave direction did not differ for AF type, nor for patients with or without acute AF termination by ablation (p=NS).
Conclusions:
In this study of patients with various types of AF, a novel AI-based approach showed that AF vectors indicating waves exiting the PVs predicted , clinical phenotypes, particularly patients with successful ablation targeting the PVs.
More abstracts on this topic:
Both electrical isolation and lesion homogeneity should be focused: evidence from repeat atrial fibrillation ablation
Li Jiaju, Tian Aiju, Jia Yuhe, Yao Yan
Age-stratified Monogenic and Polygenic Contributions for Atrial Fibrillation in the All of Us Research ProgramChen Zhanlin, Gordon Adam, Webster Gregory