Final ID: Mo4038
Demographic and regional disparities in cerebrovascular disease mortality among adult patients with pre-existing atherosclerosis in the United States from 1999-2020
Abstract Body (Do not enter title and authors here):
Introduction
Atherosclerosis (ATH) is a major risk factor for cerebrovascular disease (CEVD), with persistent mortality disparities. Our study aims to identify vulnerable regions and demographics in the US adult population with pre-existing ATH at risk of CEVD.
Methods
CDC Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) was used to access National Vital Statistics System data from 1999 to 2020. ATH-related CEVD was identified using CEVD as the underlying cause of death and ATH as a contributing cause of death. Results were presented as age-adjusted mortality rates (AAMR) per 100,000 population. Joinpoint regression was used to examine changes in trend and annual percentage change (APC).
Results
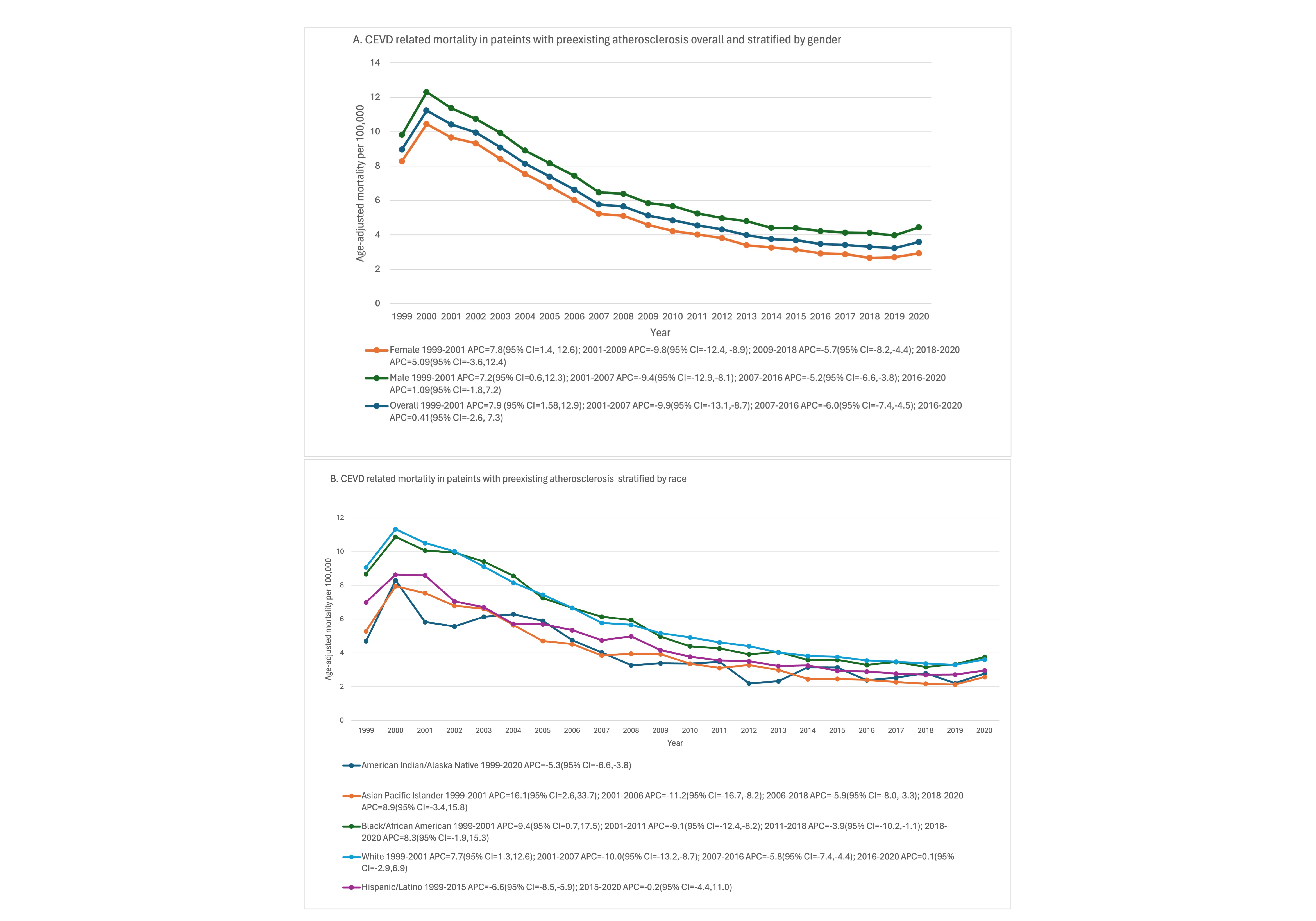
A total of 325,408 CEVD occurred in patients with ATH from 1999 to 2020 (AAMR = 6.9, 95% CI: 6.8-7). Increased mortality rates were observed in males (AAMR = 6.3) as compared to females (AAMR = 5.1) (Figure, Panel A). AAMRs were highest in Non-Hispanic Whites [NHW] (5.7, 95% CI: 5.7 - 5.8), followed by non-Hispanic blacks [NHB] (5.5, 95% CI: 5.4 - 5.5), Hispanics (4.1, 95% CI: 4.0 - 4.1) and non-Hispanic American Indian/Alaska Native [NH-AIAN] (3.6, 95% CI: 3.4 - 3.8). Non-Hispanic Asian/Pacific Islander [NH-API] had the lowest mortality rates (3.4, 95% CI: 3.4 - 3.5). Region-wise analysis revealed that mortality rates were highest in the West (6.4, 95% CI: 6.3-6.4) and Midwest (6.2, 95% CI: 6.1-6.2). The South reported the rate of 5.5 (95% CI: 5.5-5.6), while the Northeast had the lowest rate (4.4, 95% CI: 4.3-4.4). Mortality rates were consistently higher in rural areas (6.1, 95% CI: 6.0-6.1) compared to urban areas (5.3, 95% CI: 5.3-5.4) throughout the study period. Overall AAMR rose from 9.0 in 1999 to 10.4 in 2001, then steadily declined before increasing to 3.6 from 2016 to 2020 (APC: 0.41). After an initial decline, AAMR increased in men (APC: 1.09) from 2016 and in women (APC: 5.09) from 2018. AAMR also increased among NH-API (APC: 8.9) and NHB (APC: 8.3) from 2018 onwards, and NHW (APC: 0.1) from 2016 (Figure, Panel B).
Conclusions
Our study reveals significant mortality disparities from CEVD in patients with ATH, identifying males, NHW, and residents in the West and Midwest as particularly at increased risk. Rural areas consistently show higher mortality rates than urban areas. These findings highlight the need for targeted interventions and strategic provision of healthcare resources to improve outcomes for vulnerable populations.
Introduction
Atherosclerosis (ATH) is a major risk factor for cerebrovascular disease (CEVD), with persistent mortality disparities. Our study aims to identify vulnerable regions and demographics in the US adult population with pre-existing ATH at risk of CEVD.
Methods
CDC Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) was used to access National Vital Statistics System data from 1999 to 2020. ATH-related CEVD was identified using CEVD as the underlying cause of death and ATH as a contributing cause of death. Results were presented as age-adjusted mortality rates (AAMR) per 100,000 population. Joinpoint regression was used to examine changes in trend and annual percentage change (APC).
Results
A total of 325,408 CEVD occurred in patients with ATH from 1999 to 2020 (AAMR = 6.9, 95% CI: 6.8-7). Increased mortality rates were observed in males (AAMR = 6.3) as compared to females (AAMR = 5.1) (Figure, Panel A). AAMRs were highest in Non-Hispanic Whites [NHW] (5.7, 95% CI: 5.7 - 5.8), followed by non-Hispanic blacks [NHB] (5.5, 95% CI: 5.4 - 5.5), Hispanics (4.1, 95% CI: 4.0 - 4.1) and non-Hispanic American Indian/Alaska Native [NH-AIAN] (3.6, 95% CI: 3.4 - 3.8). Non-Hispanic Asian/Pacific Islander [NH-API] had the lowest mortality rates (3.4, 95% CI: 3.4 - 3.5). Region-wise analysis revealed that mortality rates were highest in the West (6.4, 95% CI: 6.3-6.4) and Midwest (6.2, 95% CI: 6.1-6.2). The South reported the rate of 5.5 (95% CI: 5.5-5.6), while the Northeast had the lowest rate (4.4, 95% CI: 4.3-4.4). Mortality rates were consistently higher in rural areas (6.1, 95% CI: 6.0-6.1) compared to urban areas (5.3, 95% CI: 5.3-5.4) throughout the study period. Overall AAMR rose from 9.0 in 1999 to 10.4 in 2001, then steadily declined before increasing to 3.6 from 2016 to 2020 (APC: 0.41). After an initial decline, AAMR increased in men (APC: 1.09) from 2016 and in women (APC: 5.09) from 2018. AAMR also increased among NH-API (APC: 8.9) and NHB (APC: 8.3) from 2018 onwards, and NHW (APC: 0.1) from 2016 (Figure, Panel B).
Conclusions
Our study reveals significant mortality disparities from CEVD in patients with ATH, identifying males, NHW, and residents in the West and Midwest as particularly at increased risk. Rural areas consistently show higher mortality rates than urban areas. These findings highlight the need for targeted interventions and strategic provision of healthcare resources to improve outcomes for vulnerable populations.