Final ID: Su1089
Geographic, Gender, & Racial Trends in Mortality Due to Heart Failure in Coronary Artery Disease Among Adults Aged 65 and Older in the United States, 1999-2020: A CDC WONDER Database Analysis
Abstract Body (Do not enter title and authors here): Backgrounds: Heart failure (HF) associated with coronary artery disease (CAD) is a significant contributor to mortality in the elderly population of the United States. This study examines trends in HF in CAD-related mortality among adults aged 65 and older, focusing on geographic, gender, and racial/ethnic disparities from 1999 to 2020.
Methods: A retrospective analysis was performed using the CDC WONDER database death certificates from 1999 to 2020. Age-adjusted mortality rates (AAMRs), annual percent change (APC), and average annual percentage change (AAPC) were calculated per 100,000 persons, stratified by year, sex, race/ethnicity, and geographical region.
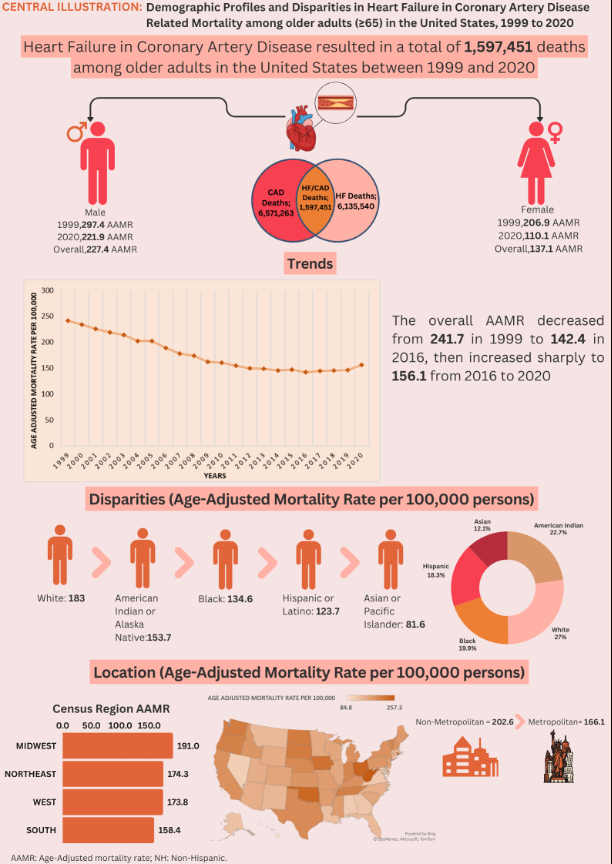
Results: Between 1999 and 2020, there were 6,571,263 deaths attributed to coronary artery disease (CAD) and 6,135,540 deaths related to Heart Failure (HF) in the US. Among adults aged 65 and older, HF in CAD caused 1,597,451 deaths, with 37.1% occurring in medical facilities and 30.3% in nursing homes. The AAMRs for HF in CAD decreased from 241.7 in 1999 to 156.2 in 2020 (AAPC: -2.23, p < 0.000001). This reduction was significant from 1999 to 2014, followed by a slight increase from 2014 to 2020. Men consistently had higher AAMRs than women (227.4 vs. 137.1), with women experiencing a more significant decline in rates (AAPC: -3.23, p < 0.000001). Racial disparities revealed the highest AAMRs among Whites (183.0), followed by American Indians/Alaska Natives (153.7), Blacks (134.6), Hispanics (123.7), and Asians/Pacific Islanders (81.6). The most significant reductions were observed in Hispanics (AAPC: -2.68, p < 0.000001). Geographically, AAMRs varied, ranging from 92.1 in Hawaii to 257.3 in West Virginia, with the Midwest showing the highest mortality (191.0). Nonmetropolitan areas exhibited higher AAMRs than metropolitan areas (202.6 vs. 166.1), although both showed moderate declines over time, more pronounced in urban areas (AAPC: -2.41, p < 0.000001).
Conclusion: The study uncovers notable variances in HF in CAD-related mortality among elderly individuals in the United States based on race, gender, and geographic location. While the decrease in AAMRs from 1999 to 2014 indicates progress in cardiovascular care, the subsequent rise from 2014 to 2020 and enduring disparities call for specific public health measures to tackle these inequalities.
Methods: A retrospective analysis was performed using the CDC WONDER database death certificates from 1999 to 2020. Age-adjusted mortality rates (AAMRs), annual percent change (APC), and average annual percentage change (AAPC) were calculated per 100,000 persons, stratified by year, sex, race/ethnicity, and geographical region.
Results: Between 1999 and 2020, there were 6,571,263 deaths attributed to coronary artery disease (CAD) and 6,135,540 deaths related to Heart Failure (HF) in the US. Among adults aged 65 and older, HF in CAD caused 1,597,451 deaths, with 37.1% occurring in medical facilities and 30.3% in nursing homes. The AAMRs for HF in CAD decreased from 241.7 in 1999 to 156.2 in 2020 (AAPC: -2.23, p < 0.000001). This reduction was significant from 1999 to 2014, followed by a slight increase from 2014 to 2020. Men consistently had higher AAMRs than women (227.4 vs. 137.1), with women experiencing a more significant decline in rates (AAPC: -3.23, p < 0.000001). Racial disparities revealed the highest AAMRs among Whites (183.0), followed by American Indians/Alaska Natives (153.7), Blacks (134.6), Hispanics (123.7), and Asians/Pacific Islanders (81.6). The most significant reductions were observed in Hispanics (AAPC: -2.68, p < 0.000001). Geographically, AAMRs varied, ranging from 92.1 in Hawaii to 257.3 in West Virginia, with the Midwest showing the highest mortality (191.0). Nonmetropolitan areas exhibited higher AAMRs than metropolitan areas (202.6 vs. 166.1), although both showed moderate declines over time, more pronounced in urban areas (AAPC: -2.41, p < 0.000001).
Conclusion: The study uncovers notable variances in HF in CAD-related mortality among elderly individuals in the United States based on race, gender, and geographic location. While the decrease in AAMRs from 1999 to 2014 indicates progress in cardiovascular care, the subsequent rise from 2014 to 2020 and enduring disparities call for specific public health measures to tackle these inequalities.
More abstracts on this topic:
Accelerometer-Measured Sedentary Behavior and Future Cardiovascular Disease
Ajufo Ezimamaka, Kany Shinwan, Ramo Joel, Churchill Timothy, Guseh James, Aragam Krishna, Ellinor Patrick, Khurshid Shaan
A Measure of Residential Segregation and Thrombo-inflammation in Black and White AmericansManogaran Erin, Cushman Mary, Kamin Mukaz Debora, Sparks Andrew, Packer Ryan, Brochu Paige, Judd Suzanne, Howard Virginia, Plante Timothy, Long Leann, Cheung Katherine