Final ID: Sa3092
Door-in to door-out time and in-hospital mortality in patients with ST-elevation myocardial infarction
Abstract Body (Do not enter title and authors here): Background: Although current guidelines recommend achieving a door-in to door-out (DIDO) time within 30 minutes for 75% of patients with ST-elevation myocardial infarction (STEMI) who require interhospital transfer for primary percutaneous coronary intervention (PCI), disparities between guidelines and clinical performance persist.
Methods: We analyzed the association between the DIDO time and in-hospital mortality using data from the Get With The Guidelines® – Coronary Artery Disease STEMI and NSTEMI Registry covering 232,935 admissions between the fourth quarter of 2019 and the third quarter of 2022. We determined the cut-off value of the DIDO time at which the odds of in-hospital mortality markedly increased by a likelihood ratio (LR) and an area under the curve (AUC) derived by generalized linear regression.
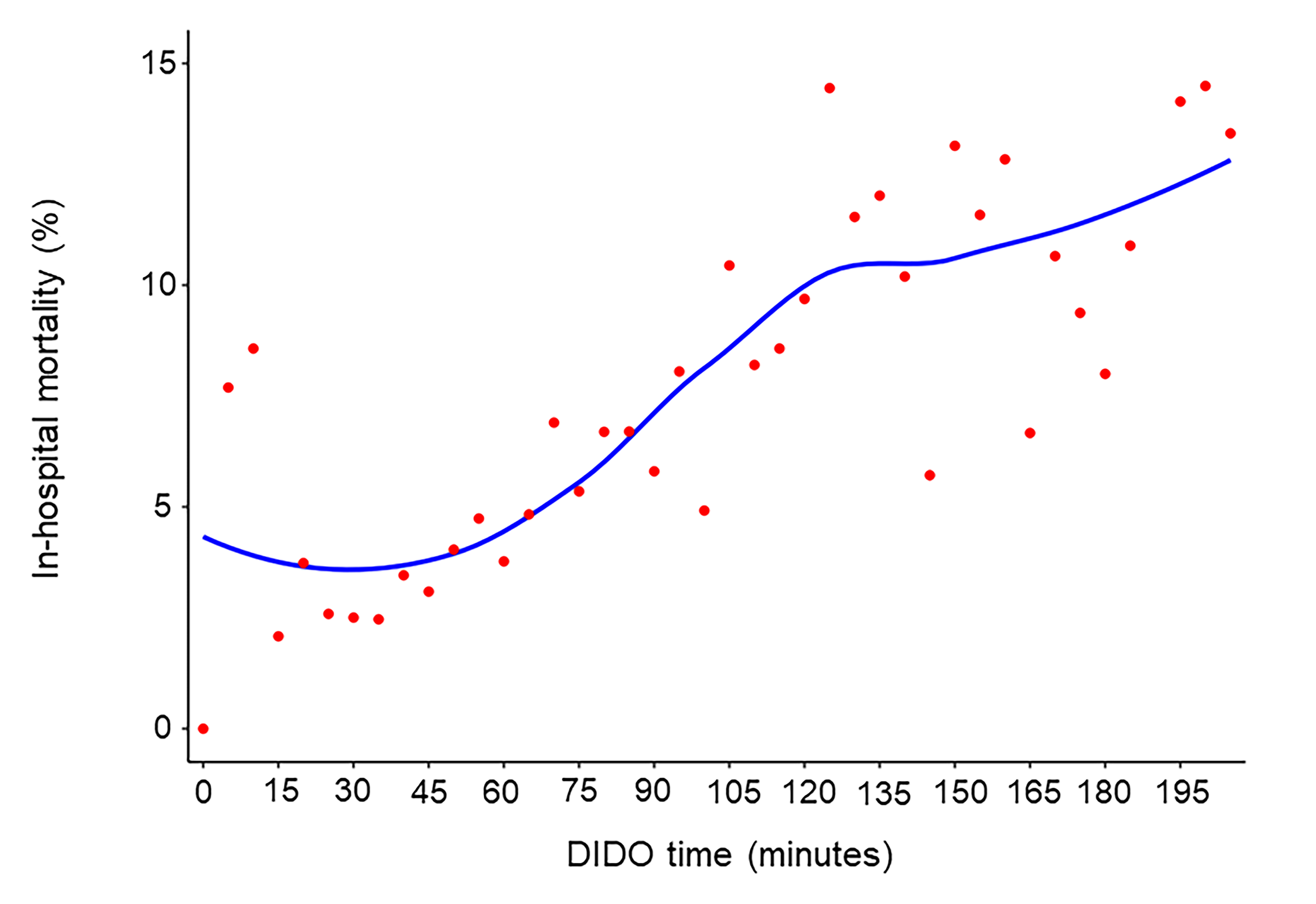
Results: Of the 103,838 patients with STEMI, 23,865 (23%) required interhospital transfer. The median DIDO time was 63 (interquartile range 43–105) minutes and was within 30 minutes in 9% of cases. Generalized linear mixed models showed that a DIDO time delay of 5 minutes was significantly associated with higher in-hospital mortality (adjusted odds ratio [OR], 1.88; 95% confidence interval [CI], 1.56–2.27; p<0.001). The LR test and AUC showed that DIDO time cut-offs at 30, 42, 63, and 93 minutes were associated with increased in-hospital mortality. Compared with a reference DIDO time of within 30 minutes, the in-hospital mortality did not significantly differ for a DIDO time from 30 to 42 minutes (adjusted OR, 1.20; 95% CI, 0.83–1.73; p=0.340), but it was significantly higher for DIDO times from 42 to 63 minutes (adjusted OR, 1.48; 95% CI, 1.06–2.06; p=0.020), 63 to 93 minutes (adjusted OR, 1.89; 95% CI, 1.36–2.63; p<0.001), and over 93 minutes (adjusted OR, 2.85; 95% CI, 2.08–3.90; p<0.001).
Conclusion: A delayed DIDO time was significantly associated with higher in-hospital mortality, particularly beyond 42 minutes.
Methods: We analyzed the association between the DIDO time and in-hospital mortality using data from the Get With The Guidelines® – Coronary Artery Disease STEMI and NSTEMI Registry covering 232,935 admissions between the fourth quarter of 2019 and the third quarter of 2022. We determined the cut-off value of the DIDO time at which the odds of in-hospital mortality markedly increased by a likelihood ratio (LR) and an area under the curve (AUC) derived by generalized linear regression.
Results: Of the 103,838 patients with STEMI, 23,865 (23%) required interhospital transfer. The median DIDO time was 63 (interquartile range 43–105) minutes and was within 30 minutes in 9% of cases. Generalized linear mixed models showed that a DIDO time delay of 5 minutes was significantly associated with higher in-hospital mortality (adjusted odds ratio [OR], 1.88; 95% confidence interval [CI], 1.56–2.27; p<0.001). The LR test and AUC showed that DIDO time cut-offs at 30, 42, 63, and 93 minutes were associated with increased in-hospital mortality. Compared with a reference DIDO time of within 30 minutes, the in-hospital mortality did not significantly differ for a DIDO time from 30 to 42 minutes (adjusted OR, 1.20; 95% CI, 0.83–1.73; p=0.340), but it was significantly higher for DIDO times from 42 to 63 minutes (adjusted OR, 1.48; 95% CI, 1.06–2.06; p=0.020), 63 to 93 minutes (adjusted OR, 1.89; 95% CI, 1.36–2.63; p<0.001), and over 93 minutes (adjusted OR, 2.85; 95% CI, 2.08–3.90; p<0.001).
Conclusion: A delayed DIDO time was significantly associated with higher in-hospital mortality, particularly beyond 42 minutes.
More abstracts on this topic:
Artificial Intelligence ECG-Extracted Features Predict Microvascular Obstruction in ST-segment Elevation Myocardial Infarction
Traverse Jay, Meyers Pendell, Sharkey Scott, Schwager Sarah, Stanberry Larissa, Herman Robert
A Randomized Clinical Trial Evaluating Vitamin D Normalization on Major Adverse Cardiovascular-Related Events Among Acute Coronary Syndrome Patients: The TARGET-D TrialMay Heidi, Colipi Dominique, Whiting Tyler, Muhlestein Joseph, Le Viet, Anderson Jeffrey, Babcock Daniel, Wayman Libby, Bair Tami, Knight Stacey, Knowlton Kirk, Iverson Leslie