Final ID: Su4011
Efficacy of Sodium Glucose Cotransporter 2 Inhibitors In Patients With Acute Myocardial Infarction: A Meta-Analysis of Randomized Controlled Trials
Abstract Body (Do not enter title and authors here): Background
Sodium-glucose cotransporter 2 (SGLT2) inhibitors improve cardiovascular outcomes in patients with or without type 2 diabetes and heart failure (HF). However, studies have shown conflicting evidence regarding their efficacy in patients following acute myocardial infarction (MI). We conducted a systematic review and meta-analysis to synthesize the available evidence regarding the effectiveness of SGLT2 inhibitors in MI.
Methods
A systematic literature search was conducted using PubMed/MEDLINE, the Cochrane Library, and Embase databases to identify randomized controlled trials (RCTs) that compared clinical outcomes of SGLT2 inhibitors with placebo following MI. We conducted the statistical analysis using RevMan, version 5.4, and pooled risk ratios (RRs) along the corresponding 95% confidence interval (CI) for all outcomes. The quality of evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology.
Results
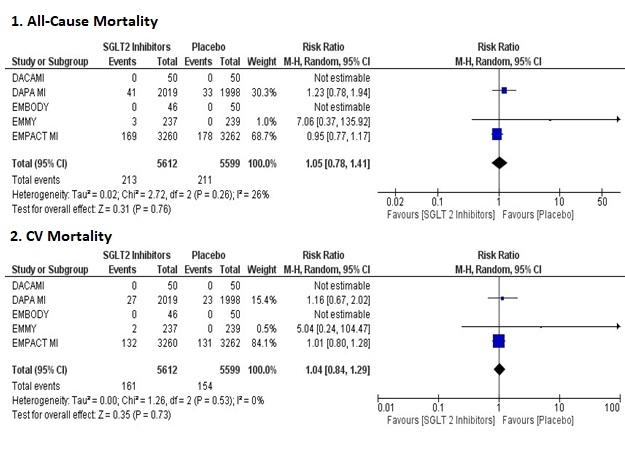
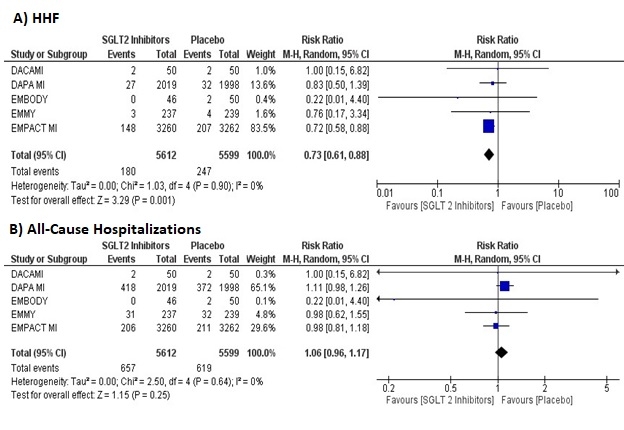
Five RCTs reporting data for 11,211 patients were included in our study. Our pooled analysis showed that SGLT2 inhibitors significantly reduced the risk of hospitalizations for heart failure (HHF) (RR = 0.76, 95% CI: 0.61-0.88, p = 0.001; high certainty). In terms of absolute effects, this translated to 12 fewer HHF per 1,000 patients who received SGLT2 inhibitors compared with the placebo (absolute risk difference 12 (95% CI 17 to 5) fewer per 1000 patients) in patients with MI. However, the risk of all-cause mortality (RR = 1.05, 95% CI: 0.78-1.41, p = 0.76; high certainty), cardiovascular (CV) mortality (RR = 1.04, 95% CI = 0.84-1.29, p = 0.73; high certainty), and all-cause hospitalizations (RR = 1.06, 95% CI: 0.96-1.17, p = 0.25; high certainty) remained comparable across the two groups.
Conclusion
SGLT2 inhibitors reduce HHF without affecting all-cause mortality, CV mortality, and all-cause hospitalizations. However, further evidence is required to reach a definitive conclusion.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors improve cardiovascular outcomes in patients with or without type 2 diabetes and heart failure (HF). However, studies have shown conflicting evidence regarding their efficacy in patients following acute myocardial infarction (MI). We conducted a systematic review and meta-analysis to synthesize the available evidence regarding the effectiveness of SGLT2 inhibitors in MI.
Methods
A systematic literature search was conducted using PubMed/MEDLINE, the Cochrane Library, and Embase databases to identify randomized controlled trials (RCTs) that compared clinical outcomes of SGLT2 inhibitors with placebo following MI. We conducted the statistical analysis using RevMan, version 5.4, and pooled risk ratios (RRs) along the corresponding 95% confidence interval (CI) for all outcomes. The quality of evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology.
Results
Five RCTs reporting data for 11,211 patients were included in our study. Our pooled analysis showed that SGLT2 inhibitors significantly reduced the risk of hospitalizations for heart failure (HHF) (RR = 0.76, 95% CI: 0.61-0.88, p = 0.001; high certainty). In terms of absolute effects, this translated to 12 fewer HHF per 1,000 patients who received SGLT2 inhibitors compared with the placebo (absolute risk difference 12 (95% CI 17 to 5) fewer per 1000 patients) in patients with MI. However, the risk of all-cause mortality (RR = 1.05, 95% CI: 0.78-1.41, p = 0.76; high certainty), cardiovascular (CV) mortality (RR = 1.04, 95% CI = 0.84-1.29, p = 0.73; high certainty), and all-cause hospitalizations (RR = 1.06, 95% CI: 0.96-1.17, p = 0.25; high certainty) remained comparable across the two groups.
Conclusion
SGLT2 inhibitors reduce HHF without affecting all-cause mortality, CV mortality, and all-cause hospitalizations. However, further evidence is required to reach a definitive conclusion.
More abstracts on this topic:
A Rare Cause of a Classic Presentation of NSTEMI: Case of 39-Year-Old Female with Hypothyroidism Induced Myocarditis
Quadri Fayz, Qazi Mariam, Teague Taylor
A Perfect Storm: Simultaneous Pulmonary Embolism, STEMI, and Stroke via Paradoxical Embolism in a Hospitalized Patient on DVT ProphylaxisKhan Abdul Allam, Thukral Jatin, Elgabry Ibrahim, Lamp Garron