Final ID: Sa2013
Reducing Blood Product Waste in a Pediatric Cardiac Catheterization Laboratory – A Quality Improvement Initiative
Transfusion can be a life-saving intervention, however routine pre-procedural blood products frequently go unused. Recent national blood product shortages highlight the importance of blood product stewardship. In our pediatric cardiac catheterization laboratory (PCCL), packed red blood cells (pRBCs) were ordered prior to all cases. These units are rarely transfused and sometimes cannot be reallocated, resulting in waste. As a quality improvement project, we set a primary aim to reduce the percentage of monthly pRBC waste from a baseline mean of 7.4% to <5% over 12 months.
Methods:
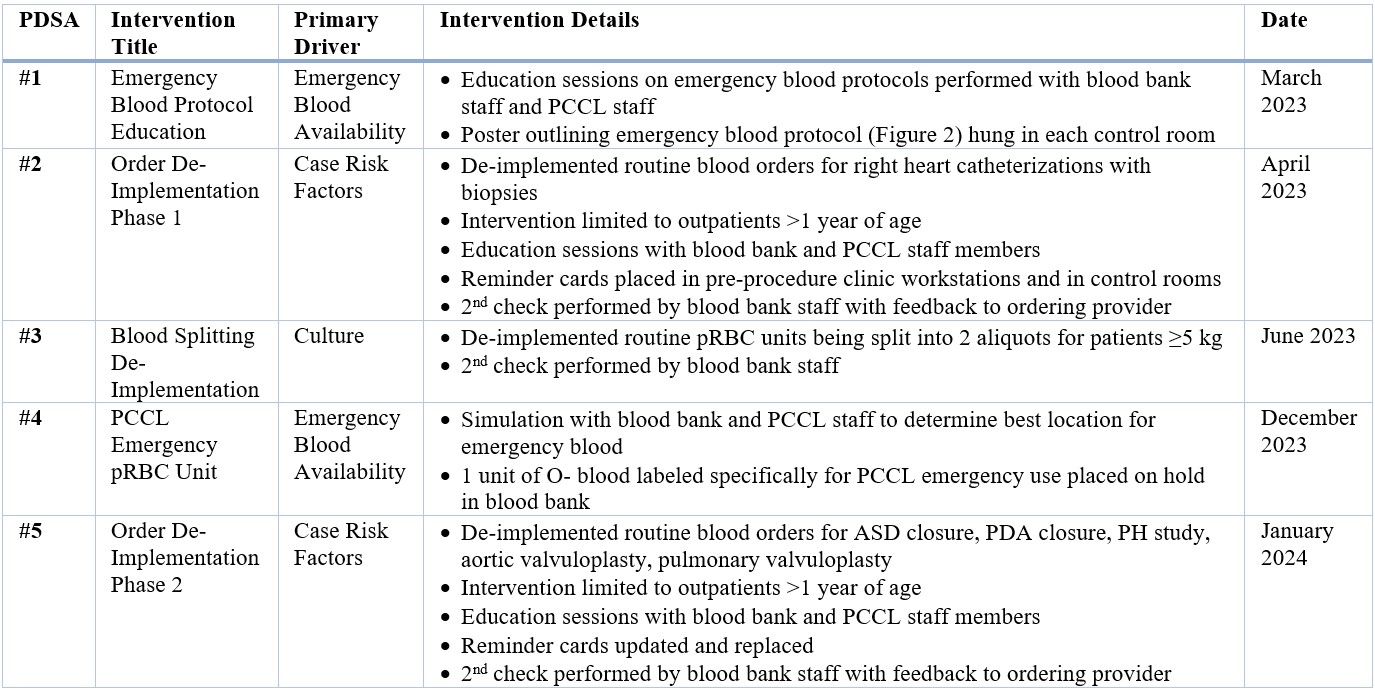
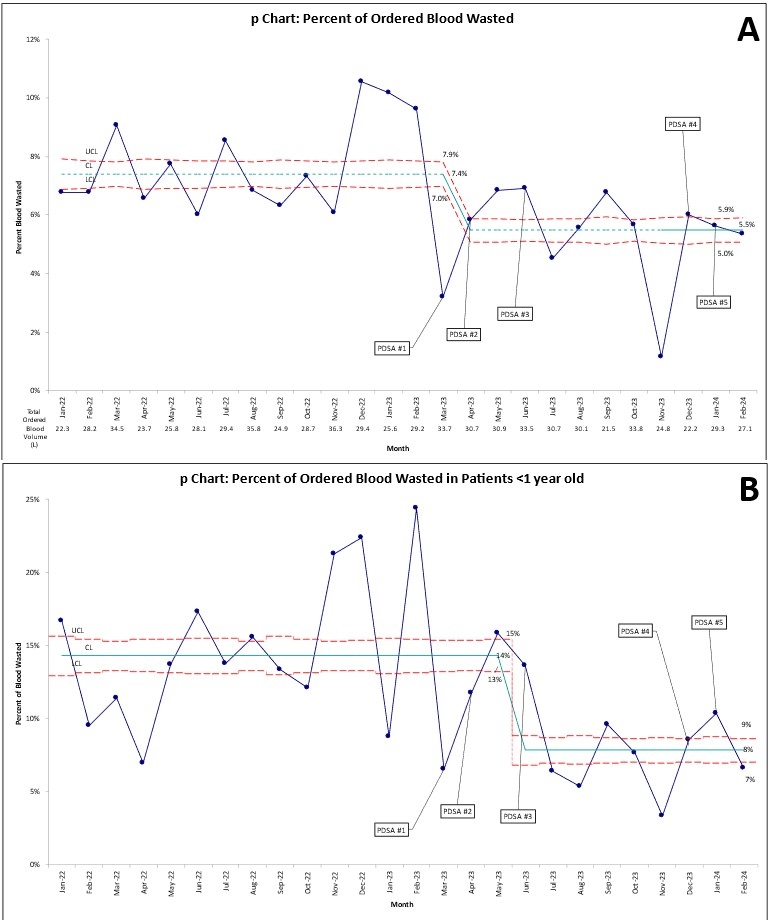
Baseline data on all cardiac catheterization cases, excluding electrophysiology, lymphatic, and hybrid cases, were collected from 1/1/2022 to 2/28/2023. Interventions (Table 1) were implemented and outcomes measured from 3/1/2023 to 3/31/2024. Primary outcome measures were monthly percentage of blood wasted, and percent of unused pRBC orders. Emergency blood product activation was measured as a balancing metric. Statistical process control charts were used to display and analyze data.
Results:
During the intervention period 1,318 cases were performed of which 32% met low-risk criteria for pRBC order de-implementation. The percent of blood that was subsequently wasted was reduced from 7.4% to 5.5% (Figure 1A), primarily driven by the reduction in the anecdotal practice of pRBC unit splitting in patients <1 year old (Figure 1B). The percent of unused pRBC orders was reduced from 97% to 79% with sustained improvement following two cycles of routine blood order de-implementation for low-risk cases. No emergency blood activation occurred (0%, 97.5% CI: 0-0.28%).
Conclusion:
De-implementation of default pRBC orders for low-risk catheterization procedures and reduction in unit splitting reduced the percent of blood wasted in our PCCL, saving time and cost without compromising patient safety. A data-driven approach to blood stewardship may be broadly applicable across procedural areas.
- Morrison, Jacqueline ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Tang, Jie ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Smith, Christopher ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Callahan, Ryan ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Gillespie, Matthew ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Rome, Jonathan ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Hehir, David ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- O'byrne, Michael ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Zedalis, Jacqueline ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Parrish, Benjamin ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Goenaga Diaz, Eduardo ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- David, Friedman ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Hawkins, Jaleah ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Shah, Farzana ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Basu, Sharna ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Ryan, Edith ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
Meeting Info:
Session Info:
Pediatric Invasive and Surgical Techniques and Outcomes
Saturday, 11/16/2024 , 10:30AM - 11:30AM
Abstract Poster Session
More abstracts on this topic:
Abuzeid Wael, Shuvy Mony, Cantor Warren, Mehta Shamir, Fam Neil, Abdel-qadir Husam, Sacoransky Ethan, Czarnecki Andrew, Ke Danny Yu Jia, Teng Carolyn, Dave Prasham, Osten Mark, Zile Brigita, Wang Xuesong
Afferent Rapid Response Limb Failure Prior to Non-ICU In-Hospital Cardiac Arrest and Associated In-Hospital MortalityShipley Kipp, Shifrin Megan, Snarskis Connor, Weavind Liza
More abstracts from these authors:
Rastogi Radhika, Ravishankar Chitra, Biko David, Vaiyani Danish, Goldberg David, Gupta Mudit, Zweben Bari, Joyce Jeremiah, Shustak Rachel, Schreier Matthew, Pinto Erin, Smith Christopher, Dori Yoav, Dewitt Aaron
Decision-Making at the Time of Fontan Completion: When and How to Decompress the Lymphatic SystemSmith Christopher, Rome Jonathan