Final ID: Mo4042
A Case of Recurrent Neurocardiogenic Syncope in a COVID-19 Patient
Abstract Body (Do not enter title and authors here): Background: COVID-19 infection has been associated with a broad range of clinical manifestations. There are very few reported cases of COVID-19 patients presenting with syncope as an initial symptom. We present an extraordinary case of recurrent neurocardiogenic syncope in a COVID-19 patient.
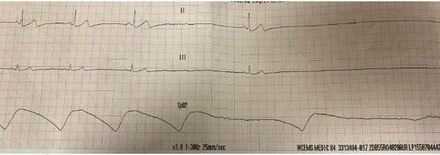
Case: A 66-year-old male presented after experiencing two episodes of syncope. He denied any prodromal or anginal symptoms. His medications included propranolol 10 mg twice daily for essential tremors. He had no family history of unexplained syncope or sudden cardiac death. He was hemodynamically stable and had one episode of fever at 102°F. Telemetry recording showed vagal-mediated sinus arrest and pauses without escape. Blood work showed normal cell counts, electrolytes, thyroid-stimulating hormone, and erythrocyte sedimentation rate, with a slightly elevated C-reactive protein of 22.2 mg/L. He tested positive for COVID-19 and had negative Lyme and Ehrlichia serologies.
Decision Making: Due to symptomatic long sinus pauses, propranolol was discontinued, and he received a temporary pacemaker set at 50 beats per minute (bpm). He had another syncopal episode while being paced at 50 bpm, suggesting a neurocardiogenic mechanism, so the pacing rate was increased to 70 bpm. An echocardiogram showed a normal ejection fraction without any significant valvular disease. The syncope was determined to be vasovagal due to autonomic dysfunction in the setting of COVID-19. After 72 hours without further syncope, the temporary pacemaker was removed, and he was discharged home with an implantable loop recorder (ILR). A one-month follow-up showed no syncope, and ILR interrogation showed no bradycardia or pauses.
Conclusion: Neurocardiogenic syncope with prolonged asystole and sinus pauses is an uncommon presentation of COVID-19 infection. The clinical course of autonomic dysfunction following COVID-19 is not very clear, and monitoring with an ILR is reasonable before considering permanent pacemaker implantation.
Case: A 66-year-old male presented after experiencing two episodes of syncope. He denied any prodromal or anginal symptoms. His medications included propranolol 10 mg twice daily for essential tremors. He had no family history of unexplained syncope or sudden cardiac death. He was hemodynamically stable and had one episode of fever at 102°F. Telemetry recording showed vagal-mediated sinus arrest and pauses without escape. Blood work showed normal cell counts, electrolytes, thyroid-stimulating hormone, and erythrocyte sedimentation rate, with a slightly elevated C-reactive protein of 22.2 mg/L. He tested positive for COVID-19 and had negative Lyme and Ehrlichia serologies.
Decision Making: Due to symptomatic long sinus pauses, propranolol was discontinued, and he received a temporary pacemaker set at 50 beats per minute (bpm). He had another syncopal episode while being paced at 50 bpm, suggesting a neurocardiogenic mechanism, so the pacing rate was increased to 70 bpm. An echocardiogram showed a normal ejection fraction without any significant valvular disease. The syncope was determined to be vasovagal due to autonomic dysfunction in the setting of COVID-19. After 72 hours without further syncope, the temporary pacemaker was removed, and he was discharged home with an implantable loop recorder (ILR). A one-month follow-up showed no syncope, and ILR interrogation showed no bradycardia or pauses.
Conclusion: Neurocardiogenic syncope with prolonged asystole and sinus pauses is an uncommon presentation of COVID-19 infection. The clinical course of autonomic dysfunction following COVID-19 is not very clear, and monitoring with an ILR is reasonable before considering permanent pacemaker implantation.
More abstracts on this topic:
Bilateral Vertebral Artery Stenosis and Severe Aortic Valve Stenosis Trigger Functional Hypotension With Neurologic Collapse and Syncope
Kilic Abdullah, Waheed Tallha, Ghani Samrah, Soliman Isaac, Armstrong David
Brash Syndrome Requiring Permanent Pacemaker: A Case ReportBhatt Nilay, Mrad Yves Najm, Gupta Shivam, Dickey Curtis