Final ID: MDP356
Muscle Quality Defines Sarcopenic Obesity in Older Adults In Association with Cardiac Function
Abstract Body (Do not enter title and authors here): Background
Obesity phenotypes are increasingly used to define cardiovascular diseases (CVD) risks. Age-related deteriorations in skeletal muscle function have ignited interest in the co-occurrence of sarcopenia and obesity in older adults. However, the traditional definition of sarcopenia (low appendicular skeletal mass [ASM] and handgrip strength [HGS]) may lead to underdiagnosis of sarcopenic obesity (SO) in overweight individuals (due to higher muscle mass). To address this enigma, we evaluated the use of muscle quality (MQ), as an alternative metric for SO, in association with cardiac function.
Methods
Community older adults without CVD were prospectively annotated for skeletal mass, HGS and cardiac function via bioimpedance analysis, dynamometer, and simultaneous acquisition of echocardiography respectively. Sarcopenia was defined by low ASM and low HGS. Low MQ (HGS divided by upper body ASM) was defined by males<5.76kg/kg and females<5.475kg/kg. Aerobic capacity (VO2 max,ml/kg/min) was computed by a physical activity prediction model. Mitral early diastolic inflow velocity to early diastolic annular tissue velocity (E/e’) and early to late diastolic inflow velocity (E/A) ratios were recorded.
Results
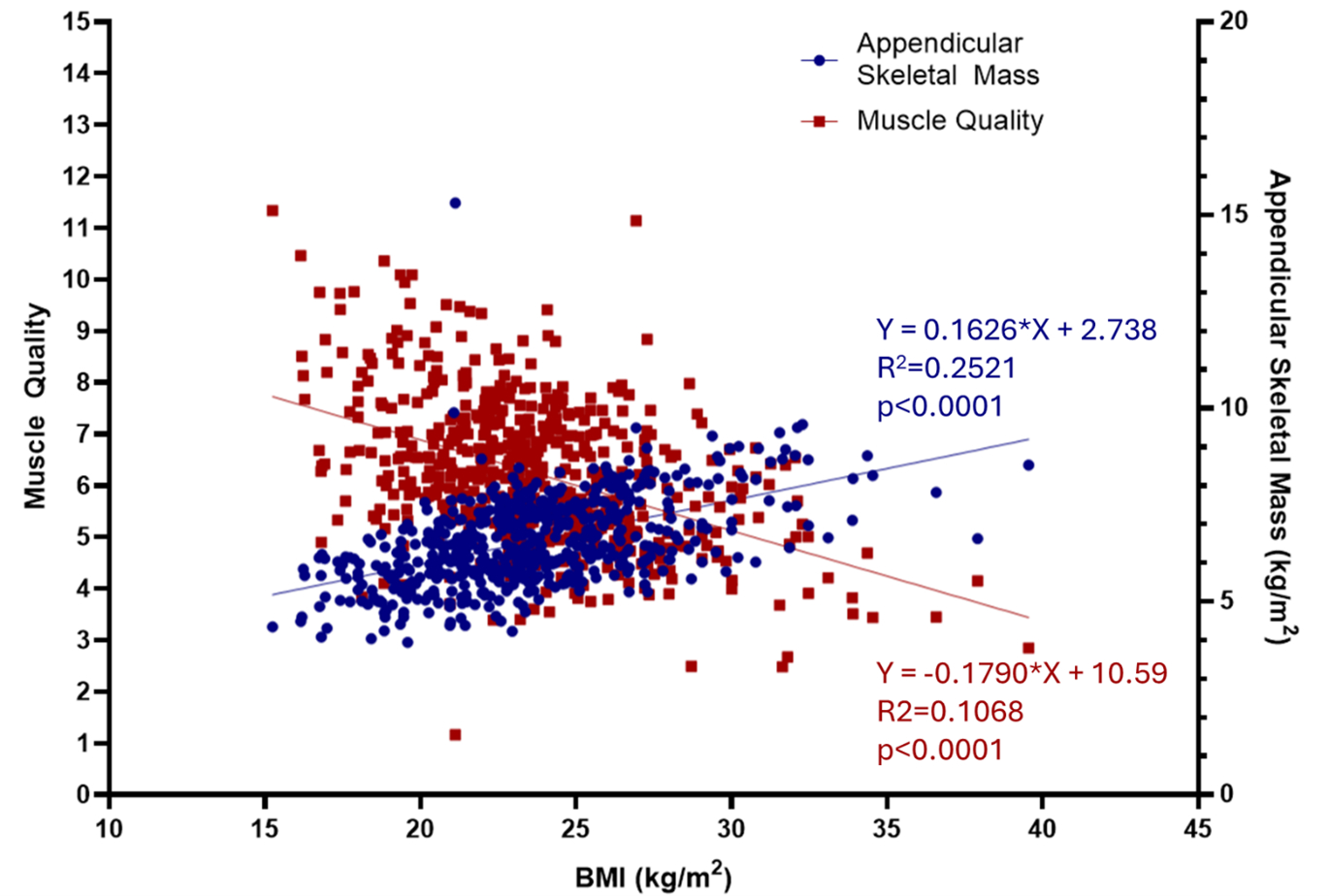
Overall, low MQ was prevalent (34.3%) in n=574 participants (59% females), but only 17.4% fulfilled sarcopenia diagnosis. Higher BMI correlated with higher ASM but lower MQ (Fig 1). Low MQ prevalence was higher in the obese compared to the non-obese (64.7% vs 30.2%, p<0.0001). Low MQ group was significantly older (69.0±10.4 vs 64.8±14.0 years, p<0.0001), had higher prevalence of dyslipidemia (49.2% vs 40.9% p=0.002) and hypertension (45.2% vs 39.3% p<0.0001) than the normal MQ group. The low MQ group had greater left ventricular mass (129±45 vs 114±44, grams, p<0.0001), left atrial volumes (37±14 vs 33±13, ml, p=0.001), and demonstrated a greater degree of diastolic dysfunction (lower E/A (0.89±0.28 vs 1.1±0.49, p<0.0001 and higher E/e’(8.63±2.42 vs 8.00±2.58, p=0.005), compared to the high MQ. VO2 max was lower in low MQ group (33±5.7 vs 36±6.7, p<0.0001). By regression, low MQ was associated with E/A (β=-0.119, adjusted p<0.0001) and VO2 max (β=-0.137, p<0.0001) (Table 1).
Conclusion
Muscle quality is a useful metric of muscle function for sarcopenia in obese older adults. The associations between low MQ with diastolic dysfunction and reduced aerobic capacity corroborate the clinical impact of MQ as a defining metric of sarcopenia in obesity.
Obesity phenotypes are increasingly used to define cardiovascular diseases (CVD) risks. Age-related deteriorations in skeletal muscle function have ignited interest in the co-occurrence of sarcopenia and obesity in older adults. However, the traditional definition of sarcopenia (low appendicular skeletal mass [ASM] and handgrip strength [HGS]) may lead to underdiagnosis of sarcopenic obesity (SO) in overweight individuals (due to higher muscle mass). To address this enigma, we evaluated the use of muscle quality (MQ), as an alternative metric for SO, in association with cardiac function.
Methods
Community older adults without CVD were prospectively annotated for skeletal mass, HGS and cardiac function via bioimpedance analysis, dynamometer, and simultaneous acquisition of echocardiography respectively. Sarcopenia was defined by low ASM and low HGS. Low MQ (HGS divided by upper body ASM) was defined by males<5.76kg/kg and females<5.475kg/kg. Aerobic capacity (VO2 max,ml/kg/min) was computed by a physical activity prediction model. Mitral early diastolic inflow velocity to early diastolic annular tissue velocity (E/e’) and early to late diastolic inflow velocity (E/A) ratios were recorded.
Results
Overall, low MQ was prevalent (34.3%) in n=574 participants (59% females), but only 17.4% fulfilled sarcopenia diagnosis. Higher BMI correlated with higher ASM but lower MQ (Fig 1). Low MQ prevalence was higher in the obese compared to the non-obese (64.7% vs 30.2%, p<0.0001). Low MQ group was significantly older (69.0±10.4 vs 64.8±14.0 years, p<0.0001), had higher prevalence of dyslipidemia (49.2% vs 40.9% p=0.002) and hypertension (45.2% vs 39.3% p<0.0001) than the normal MQ group. The low MQ group had greater left ventricular mass (129±45 vs 114±44, grams, p<0.0001), left atrial volumes (37±14 vs 33±13, ml, p=0.001), and demonstrated a greater degree of diastolic dysfunction (lower E/A (0.89±0.28 vs 1.1±0.49, p<0.0001 and higher E/e’(8.63±2.42 vs 8.00±2.58, p=0.005), compared to the high MQ. VO2 max was lower in low MQ group (33±5.7 vs 36±6.7, p<0.0001). By regression, low MQ was associated with E/A (β=-0.119, adjusted p<0.0001) and VO2 max (β=-0.137, p<0.0001) (Table 1).
Conclusion
Muscle quality is a useful metric of muscle function for sarcopenia in obese older adults. The associations between low MQ with diastolic dysfunction and reduced aerobic capacity corroborate the clinical impact of MQ as a defining metric of sarcopenia in obesity.
More abstracts on this topic:
Detecting Myosteatosis-Related Low Physical Function in Heart Failure Patients Using Abdominal Computed Tomography and Plasma Amino Acid Profile
Kawaharata Wataru, Nishikawa Ryo, Fujito Takefumi, Nobutaka Nagano, Furuhashi Masato, Kouzu Hidemichi, Ogura Keishi, Yano Toshiyuki, Katano Satoshi, Nagaoka Ryohei, Numazawa Ryo, Yamano Kotaro, Ohori Katsuhiko
Administration of the Recombinant Activated Protein C Rescues the Cardiac Vulnerability to Ischemic Insults in Aging through Modulating Inflammatory Response during Ischemia and ReperfusionSlotabec Lily, Rouhi Nadiyeh, Seale Blaise, Wang Hao, Filho Fernanda, Adenawoola Michael, Li Ji