Final ID: Mo4127
Partial versus Full ECMO Support in Combined Cardiogenic and Septic Shock – ELSO Registry Analysis
Abstract Body (Do not enter title and authors here): Background
There remains paucity of data on patient outcomes with combined cardiogenic and septic shock requiring veno-arterial extracorporeal membrane oxygenation (VA-ECMO) support. While guidelines exist on target VA-ECMO flow in cardiogenic shock patients, optimal (partial versus full) flow in combined shock remains largely unknown.
Methods
We queried the Extracorporeal Life Support Organization registry to identify patients in combined cardiogenic and septic shock supported with VA-ECMO between 2017 and 2022. Patients were categorized into either partial or full ECMO support based on ECMO flow at 24 hours indexed to body surface area. Partial support was defined as < 2.2 liters/m2 while full support was ≥2.2 liters/m2. Patients with other forms of mechanical circulatory support, VA-ECMO as bridge to advanced therapies or discharged on VA-ECMO were excluded from the analysis. Primary outcome of interest was survival to discharge. Baseline characteristics including center volumes and Charlson co-morbidity index were compared between survivors and non survivors. Predictors of mortality were identified using multivariable logistical regression model.
Results
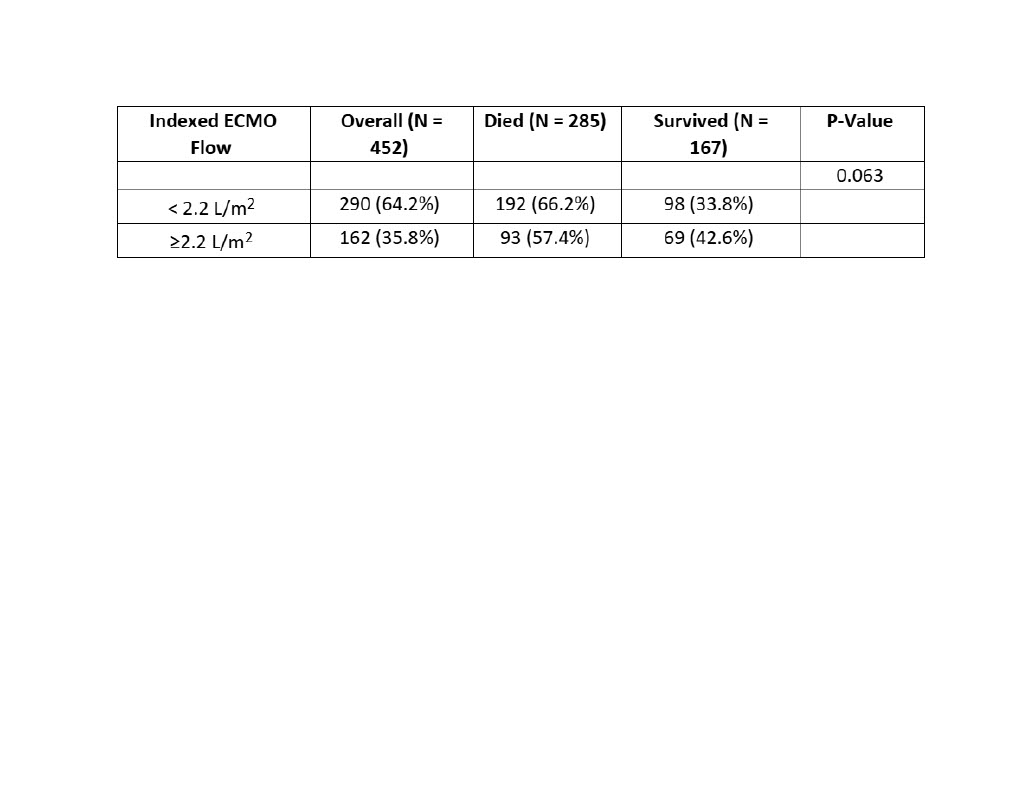
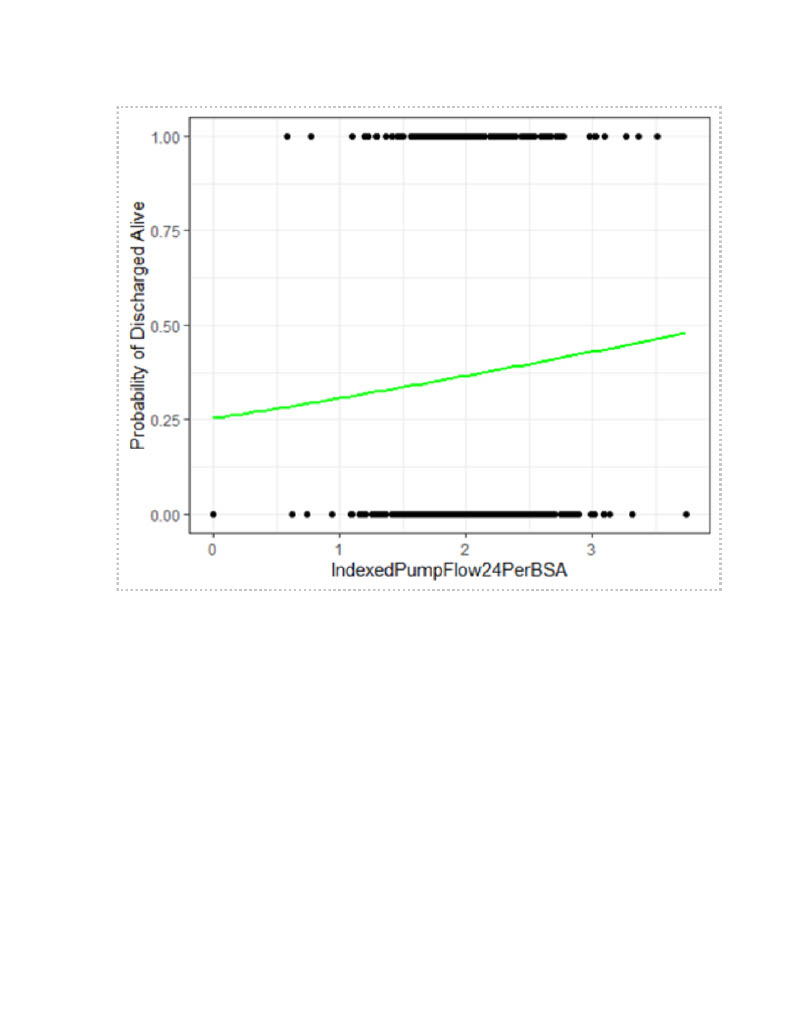
A total of 452 patients with combined shock supported with VA-ECMO were identified. Overall mortality was 63%. Patients that survived to discharge were younger (46.3 vs 53 years, p < 0.001) and had lower BMI (29.3 vs 31.1, p = 0.041), Charlson co-morbidity index (1.4 vs 2.0, p = 0.01) and rates of pre-ECMO cardiac arrest (28.7% vs 39.4%, p = 0.023). Survivors were also more likely to be at high [> 25 ECMO runs per year] volume centers compared to low [≤ 10 ECMO runs per year] volume centers (62.3% vs 20.4%, p = 0.04). Patients receiving full ECMO support had a higher likelihood of survival to discharge than partial support (42.6% vs 33.8%, p = 0.063), although it did not reach statistical significance. [Table 1] Indexed VA-ECMO flow at 24 hours was also associated with improved outcomes when assessed as continuous variable. [ Figure 1] Advanced age [aOR 1.02, 95% CI 1.01-1.04, p < 0.001], pre-ECMO cardiac arrest [aOR 1.71, 95% CI 1.11-2.65, p = 0.016] and baseline Charlson co-morbidity index [aOR 1.13, 95% CI 1.01-1.28, p = 0.043] were all associated with increased mortality after adjustment for baseline differences.
Conclusion
Mortality among patients requiring VA-ECMO for combined cardiogenic and septic shock is high. Full circulatory support may be associated with improved survival in this cohort.
There remains paucity of data on patient outcomes with combined cardiogenic and septic shock requiring veno-arterial extracorporeal membrane oxygenation (VA-ECMO) support. While guidelines exist on target VA-ECMO flow in cardiogenic shock patients, optimal (partial versus full) flow in combined shock remains largely unknown.
Methods
We queried the Extracorporeal Life Support Organization registry to identify patients in combined cardiogenic and septic shock supported with VA-ECMO between 2017 and 2022. Patients were categorized into either partial or full ECMO support based on ECMO flow at 24 hours indexed to body surface area. Partial support was defined as < 2.2 liters/m2 while full support was ≥2.2 liters/m2. Patients with other forms of mechanical circulatory support, VA-ECMO as bridge to advanced therapies or discharged on VA-ECMO were excluded from the analysis. Primary outcome of interest was survival to discharge. Baseline characteristics including center volumes and Charlson co-morbidity index were compared between survivors and non survivors. Predictors of mortality were identified using multivariable logistical regression model.
Results
A total of 452 patients with combined shock supported with VA-ECMO were identified. Overall mortality was 63%. Patients that survived to discharge were younger (46.3 vs 53 years, p < 0.001) and had lower BMI (29.3 vs 31.1, p = 0.041), Charlson co-morbidity index (1.4 vs 2.0, p = 0.01) and rates of pre-ECMO cardiac arrest (28.7% vs 39.4%, p = 0.023). Survivors were also more likely to be at high [> 25 ECMO runs per year] volume centers compared to low [≤ 10 ECMO runs per year] volume centers (62.3% vs 20.4%, p = 0.04). Patients receiving full ECMO support had a higher likelihood of survival to discharge than partial support (42.6% vs 33.8%, p = 0.063), although it did not reach statistical significance. [Table 1] Indexed VA-ECMO flow at 24 hours was also associated with improved outcomes when assessed as continuous variable. [ Figure 1] Advanced age [aOR 1.02, 95% CI 1.01-1.04, p < 0.001], pre-ECMO cardiac arrest [aOR 1.71, 95% CI 1.11-2.65, p = 0.016] and baseline Charlson co-morbidity index [aOR 1.13, 95% CI 1.01-1.28, p = 0.043] were all associated with increased mortality after adjustment for baseline differences.
Conclusion
Mortality among patients requiring VA-ECMO for combined cardiogenic and septic shock is high. Full circulatory support may be associated with improved survival in this cohort.
More abstracts on this topic:
Cardiopulmonary Bypass and Aortic Cross-Clamp Times as Predictors of Outcomes in ECMO-Supported Cardiotomy Patients
Banker Himanshi, Sarangi Swapna, Jena Anek, Seelhammer Troy, Bohman John, Haney John, Chaudhary Sanjay, Guru Pramod
Admission Cell-free DNA Predicts Cardiogenic Shock Progression and In-Hospital MortalityPark Ashley, Kong Hyesik, Andargie Temesgen, Jang Moon, Solomon Michael, Brusca Samuel, Barnett Christopher, Obrien Connor, Agbor-enoh Sean