Final ID: Su4023
Outcomes of Heart Failure with Preserved Ejection Fraction Patients With Concurrent Opioid Use: Insights From the National Inpatient Sample
Abstract Body (Do not enter title and authors here): Background: Opioid use has increased significantly in the past few decades, impacting cardiac and non-cardiac patients. As heart failure with preserved ejection fraction (HFpEF) comprises half of all heart failure cases, understanding its management and effect on outcomes is crucial. This study aims to evaluate the outcomes of chronic opioid therapy on HFpEF patients.
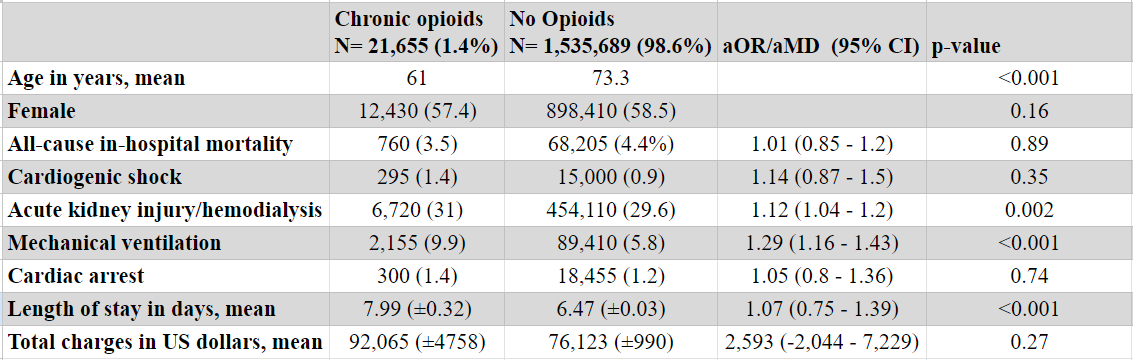
Methods: Studying the National Inpatient Sample (2016-2020), we identified adult HFpEF patients using the appropriate ICD-10 codes -after excluding patients with end-stage renal disease (ESRD)- and compared outcomes between chronic opioid users and non-users. Multivariate logistic and linear regression analyses were performed, adjusting for multiple patient and hospital confounders. The primary outcome was all-cause in-hospital mortality while secondary outcomes included acute kidney injury/hemodialysis (AKI/HD), cardiogenic shock, cardiac arrest, mechanical ventilation, length of stay, and total charges.
Results: Among 1,557,344 HFpEF patients, 21,655 (1.4%) were on opioids chronically. Inpatient mortality was not significantly different between patients who were on opioids and those who were not. (adjusted odds ratio [aOR] 1.01, 95% CI 0.85 - 1.2, p=0.89). There was a non-significant increased risk of cardiogenic shock (aOR 1.14, 95% CI 0.87 - 1.5, p=0.35) and cardiac arrest (aOR 1.05, 95% CI 0.8 - 1.36, p=0.74) in patients on chronic opioids. Chronic opioids were associated with increased risk of AKI/HD (aOR 1.12, 95% CI 1.04 - 1.2, p=0.002) and mechanical ventilation (aOR 1.29, 95% CI 1.16 - 1.43, p< 0.001). Opioid use was also associated with longer hospital stay (adjusted MD [aMD] 1.07 days, 95% CI 0.75 - 1.39, p<0.001) and a non-significant increase in total charges (aMD $2,593, 95% CI -$2,044 - $7,229, p=0.27).
Conclusions: While chronic opioid use in hospitalized HFpEF patients did not significantly impact in-hospital mortality, it was associated with increased risk of other adverse events and longer hospital stay. Further research is needed to understand the impact of chronic opioid use on HFpEF patients.
Methods: Studying the National Inpatient Sample (2016-2020), we identified adult HFpEF patients using the appropriate ICD-10 codes -after excluding patients with end-stage renal disease (ESRD)- and compared outcomes between chronic opioid users and non-users. Multivariate logistic and linear regression analyses were performed, adjusting for multiple patient and hospital confounders. The primary outcome was all-cause in-hospital mortality while secondary outcomes included acute kidney injury/hemodialysis (AKI/HD), cardiogenic shock, cardiac arrest, mechanical ventilation, length of stay, and total charges.
Results: Among 1,557,344 HFpEF patients, 21,655 (1.4%) were on opioids chronically. Inpatient mortality was not significantly different between patients who were on opioids and those who were not. (adjusted odds ratio [aOR] 1.01, 95% CI 0.85 - 1.2, p=0.89). There was a non-significant increased risk of cardiogenic shock (aOR 1.14, 95% CI 0.87 - 1.5, p=0.35) and cardiac arrest (aOR 1.05, 95% CI 0.8 - 1.36, p=0.74) in patients on chronic opioids. Chronic opioids were associated with increased risk of AKI/HD (aOR 1.12, 95% CI 1.04 - 1.2, p=0.002) and mechanical ventilation (aOR 1.29, 95% CI 1.16 - 1.43, p< 0.001). Opioid use was also associated with longer hospital stay (adjusted MD [aMD] 1.07 days, 95% CI 0.75 - 1.39, p<0.001) and a non-significant increase in total charges (aMD $2,593, 95% CI -$2,044 - $7,229, p=0.27).
Conclusions: While chronic opioid use in hospitalized HFpEF patients did not significantly impact in-hospital mortality, it was associated with increased risk of other adverse events and longer hospital stay. Further research is needed to understand the impact of chronic opioid use on HFpEF patients.
More abstracts on this topic:
Acoramidis Effect on All-Cause Mortality in Patients with p.V142I (V122I) Variant ATTR-CM: Findings From the ATTRibute-CM Study
Alexander Kevin, Bhatt Kunal, Judge Daniel, Grodin Justin, Akinboboye Olakunle, Chen Chris, Tamby Jean-francois, Castano Adam, Fox Jonathan, Fontana Marianna, Gillmore Julian, Sarswat Nitasha, Grogan Martha, Solomon Scott, Davis Margot, Cuddy Sarah, Kittleson Michelle, Shah Keyur, Griffin Jan, Ruberg Frederick, Khouri Michel
A Multi-centre, Randomized, Controlled Study of External CounterPulsation for Patients with Recent Atherosclerotic Stroke (SPA)Xiong Li, Chen Xiangyan, Leung Howan, Zhu Lixia, Leung Thomas, Wong Lawrence